Secondary Medical Insurance
- What Makes Secondary Insurance Different from Supplemental Coverage
- Key Points About Secondary Medical Insurance
- Understanding Primary and Secondary Coverage Through Real Scenarios
- Best Practices for Managing Secondary Medical Insurance
- Pitfalls to Avoid When Dealing with Secondary Coverage
- Industry Applications of Secondary Medical Insurance
- Implementation Plan for Secondary Insurance Education
- Future Outlook and Trends in Secondary Medical Insurance
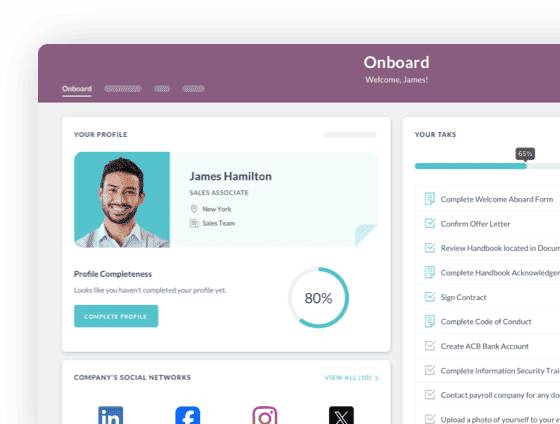
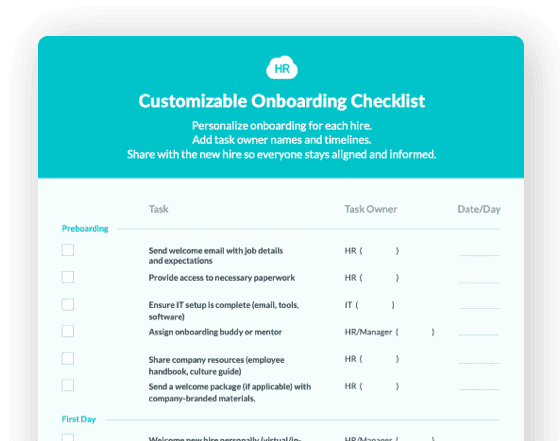
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Secondary medical insurance plays a vital role in today's complex healthcare landscape. It works alongside your primary health coverage to help reduce out-of-pocket costs and provide additional protection when medical expenses exceed your main plan's limits. Many employees find themselves with dual coverage through various life circumstances, from marriage to aging dependents, making this topic increasingly relevant for HR professionals and business leaders alike.
Understanding how secondary insurance functions is essential for anyone managing employee benefit programs or making strategic decisions about workforce compensation packages. When employees have access to two health plans, coordination of benefits determines which plan pays first and how the second plan supplements remaining costs. This process ensures that combined payments never exceed 100% of the actual medical expenses, preventing duplicate reimbursements while maximizing coverage for your team.
According to the National Association of Insurance Commissioners, coordination of benefits has become a standard industry practice that protects both employers and employees from overpayment while ensuring comprehensive medical coverage. The complexity of managing dual insurance coverage requires clear communication, proper documentation, and strategic planning from HR teams who want to help employees make the most of their available benefits.
What Makes Secondary Insurance Different from Supplemental Coverage
Secondary medical insurance is your second layer of health coverage that kicks in after your primary plan has processed a claim. Unlike supplemental insurance that pays lump sums directly to policyholders, secondary insurance coordinates with your primary carrier to cover eligible expenses that remain unpaid. This distinction matters because it affects how claims are processed, what costs get covered, and how much you ultimately pay out of pocket.
Your primary insurance acts as the first responder to any medical claim. It processes the bill according to its coverage rules, pays its portion, and sends an explanation of benefits showing what it covered. The secondary plan then reviews what remains and may cover additional costs like copays, coinsurance, or portions that exceeded your primary plan's limits. Both plans work together through a formal coordination process that ensures seamless coverage without overpayment.
Key Points About Secondary Medical Insurance
Understanding the fundamentals of secondary coverage helps HR teams guide employees through their benefit options effectively. These core concepts form the foundation of successful dual coverage management.
-
Secondary insurance never pays before your primary plan processes the claim first, regardless of which plan offers better coverage for a specific service.
-
The coordination of benefits process follows standardized rules established by state insurance commissioners to determine which plan is primary and which is secondary.
-
Employees covered under multiple plans must pay separate premiums and may face different deductibles for each policy, increasing their monthly healthcare costs.
-
According to eHealth research, the birthday rule determines primary coverage for dependent children when both parents have insurance, with the earlier birthday in the calendar year taking priority.
-
Secondary coverage typically does not pay for copays or coinsurance required by your primary plan unless specifically designed to do so, leaving some out-of-pocket costs even with dual coverage.
-
Combined benefits from both plans cannot exceed 100% of the total allowable medical expenses, preventing windfall payments to patients or providers.
Understanding Primary and Secondary Coverage Through Real Scenarios
The table below illustrates how primary and secondary insurance coordinate to cover medical expenses in different common situations:
|
Scenario |
Primary Coverage |
Secondary Coverage |
Employee Responsibility |
|
Married employee covered by own employer and spouse's plan |
Employee's own employer plan |
Spouse's employer plan |
Remaining copays and deductibles from both plans |
|
Employee under 26 with own job insurance and parent's plan |
Employee's own employer plan |
Parent's plan |
Costs not covered by either plan after coordination |
|
Dependent child covered by both parents' plans |
Plan of parent with earlier birthday in year |
Plan of parent with later birthday in year |
Any remaining balance after both plans pay |
|
Retired employee with Medicare and former employer coverage |
Medicare (if 65+ and company has fewer than 20 employees) |
Former employer retiree coverage |
Medicare gaps not covered by secondary plan |
|
Employee with COBRA and new employer coverage |
New employer's active plan |
COBRA continuation coverage |
Out-of-pocket maximums from primary plan |
Best Practices for Managing Secondary Medical Insurance
Successfully navigating dual coverage requires proactive planning and clear communication between HR teams, employees, and insurance carriers. These practices help maximize benefits while minimizing administrative headaches.
Before implementing secondary insurance guidance in your organization, assess whether the added complexity provides genuine value to your workforce. Many employees find that paying two premiums outweighs the benefit of reduced copays, especially if both plans offer similar coverage limits and provider networks. Help your team members calculate their total annual healthcare costs under dual coverage scenarios versus single plan options.
Always inform both insurance carriers about the existence of other coverage as soon as possible. This transparency allows proper coordination of benefits from the start and prevents claim denials or processing delays. During employee onboarding, collect detailed information about any additional coverage team members may have through spouses, parents, or other sources. This upfront documentation streamlines future claims processing and reduces administrative burden on your HR team.
Educate employees about the claims submission sequence required for dual coverage. They must always submit claims to their primary insurance first, wait for the explanation of benefits, and then forward remaining charges to their secondary carrier with documentation from the primary plan. Provide clear written instructions and examples during benefits enrollment periods to prevent confusion and ensure proper claim handling.
Review provider networks carefully when employees have dual coverage. Each plan may have different participating doctors and hospitals, potentially limiting where employees can receive in-network care from both policies. Encourage team members to verify that their preferred healthcare providers accept both insurance plans before assuming dual coverage will work seamlessly.
Keep detailed records of all insurance cards, policy numbers, group numbers, and contact information for both carriers. When medical providers ask about insurance coverage, employees need to present both cards and specify which is primary. This simple practice prevents billing errors and speeds up the claims process for everyone involved.
Pitfalls to Avoid When Dealing with Secondary Coverage
Even well-intentioned employees and HR teams can make costly mistakes when managing dual insurance coverage. Recognizing these common errors helps you guide your workforce toward better outcomes.
Assuming secondary insurance will cover all remaining costs after the primary plan pays is a frequent misconception. Secondary plans only cover expenses that fall within their own coverage rules, meaning you might still face out-of-pocket costs even with two policies. Many employees discover too late that their secondary plan excludes certain services their primary plan also limits, leaving them responsible for significant bills.
Failing to update coordination of benefits information with both carriers leads to claim denials and payment delays. When life circumstances change through marriage, divorce, job changes, or dependent aging out of coverage, both insurance companies need immediate notification. Outdated coordination information can result in incorrect primary/secondary designations that complicate claims for months.
Neglecting to consider the total cost of dual coverage premiums against potential savings is a critical financial mistake. Adding a second plan might cost $200 monthly in additional premiums while only reducing out-of-pocket expenses by $100 annually. This math does not work in the employee's favor, yet many people maintain costly dual coverage without doing the calculations.
Choosing in-network providers for only one plan without checking the second carrier's network creates unexpected bills. When your primary plan considers a doctor in-network but your secondary plan does not, you might pay significantly more than anticipated. Always verify network status with both carriers before scheduling non-emergency care.
Missing the connection between HR compliance requirements and benefits coordination puts companies at risk. Employers must properly administer benefits enrollment, maintain accurate records, and provide clear communication about how dual coverage works. Compliance failures in benefits administration can trigger audits and penalties that far exceed any administrative time saved by incomplete processes.
Industry Applications of Secondary Medical Insurance
Secondary medical insurance plays out differently across various business sectors, reflecting the unique workforce characteristics and benefit strategies in each industry.
In healthcare organizations, many nursing staff and medical professionals maintain dual coverage because both spouses work in high-paying medical roles with comprehensive benefits. A registered nurse covered under her hospital's plan might also join her physician spouse's insurance, creating secondary coverage that helps manage high deductibles and out-of-pocket maximums. These dual-income medical families often face significant healthcare costs themselves, making the secondary insurance valuable despite higher premium costs.
Technology companies with younger workforces frequently encounter secondary insurance situations as employees under 26 remain on parental plans while also enrolling in employer-sponsored coverage. A software developer might stay on her parents' insurance for continuity while adding her new employer's plan as primary coverage. This overlap period helps young professionals transition to full independence without coverage gaps, though many eventually drop one plan to reduce costs.
Manufacturing and retail sectors with multi-location operations see secondary insurance through spousal coverage more than other industries. When both partners work full-time with benefits, coordination of benefits becomes essential for families managing healthcare costs. HR teams in these sectors must provide clear guidance during new hire onboarding about how dual coverage works and whether maintaining both plans makes financial sense for different family situations.
Implementation Plan for Secondary Insurance Education
Creating an effective secondary insurance education program helps your workforce make informed decisions about dual coverage. Follow this step-by-step approach to build knowledge and confidence among your team.
Start by auditing your current benefits communication materials to identify gaps in secondary insurance information. Review your employee handbook, benefits guides, and onboarding documentation for clarity and completeness. Many organizations assume employees understand coordination of benefits when in reality most people find the concept confusing and intimidating.
Develop clear, plain-language resources that explain how secondary insurance works using real examples from your industry. Create flowcharts showing the claims process, comparison tables illustrating cost scenarios, and FAQs addressing the most common questions your HR team receives. Avoid insurance jargon and focus on practical guidance that employees can actually use when making coverage decisions.
Schedule targeted education sessions during open enrollment periods when employees are actively thinking about their benefit choices. Offer small group workshops where people can ask questions about their specific situations without feeling rushed or confused. Consider bringing in representatives from your insurance carriers who can provide expert guidance on coordination of benefits rules.
Implement a tracking system within your HRIS to flag employees who indicate they have other coverage during enrollment. This early identification allows your benefits team to provide personalized guidance and ensure proper coordination from the start. Follow proper HR compliance protocols when collecting and storing information about employee coverage from other sources.
Create a dedicated resource within your employee portal where team members can access secondary insurance information year-round. Include contact information for both your HR team and insurance carrier representatives who can answer specific coordination questions. Regular access to reliable information reduces confusion and helps employees manage their coverage more effectively.
Establish an annual review process where employees with dual coverage confirm their coordination of benefits information with both carriers. This proactive approach prevents claim delays and ensures accurate primary/secondary designations throughout the year. Send reminders at the beginning of each calendar year when many families experience coverage changes.
Future Outlook and Trends in Secondary Medical Insurance
The landscape of secondary medical insurance continues to evolve as healthcare costs rise and workforce demographics shift. Understanding emerging trends helps HR leaders prepare for the changing needs of their organizations.
Healthcare consumerism is driving more employees to actively compare dual coverage options using sophisticated decision-support tools. Digital platforms now allow workers to model different scenarios, calculating total costs under various coverage combinations. This transparency empowers better decision making but also increases the complexity HR teams must navigate when supporting employees through the benefits selection process.
The rise of high-deductible health plans paired with health savings accounts is changing how secondary insurance fits into overall benefits strategy. More employees are discovering that supplemental accident or hospital indemnity plans provide better value than traditional secondary medical coverage for managing out-of-pocket costs. These alternative approaches to coverage gaps may reduce the prevalence of traditional dual medical insurance over time.
According to MetLife research, approximately 43 million Americans had multiple health plans in 2021, a number that continues growing as more couples maintain dual-income households with employer benefits. This trend shows no signs of slowing, meaning HR professionals must become increasingly sophisticated in managing coordination of benefits for larger portions of their workforce.
Artificial intelligence and machine learning are beginning to streamline coordination of benefits processing, potentially reducing claim delays and errors. Insurance carriers are investing heavily in technology that can automatically identify dual coverage situations and correctly process claims through both plans. This automation will make secondary insurance easier to manage for both employers and employees in the coming years.
Regulatory changes at both state and federal levels continue to refine how coordination of benefits works, particularly around Medicare interactions with employer coverage. Staying current with these evolving rules requires ongoing education and may impact how you structure benefits for employees approaching Medicare eligibility. Progressive HR teams are already building expertise in these transition scenarios to support their aging workforce effectively.
The shift toward more flexible work arrangements, including remote work and gig economy participation, is creating new secondary insurance scenarios that traditional coordination rules never anticipated. As employees increasingly hold multiple part-time positions or combine W-2 employment with independent contractor work, determining primary versus secondary coverage becomes more complex. Forward-thinking organizations are developing new frameworks to support these non-traditional employment relationships while ensuring adequate healthcare coverage for their entire workforce.
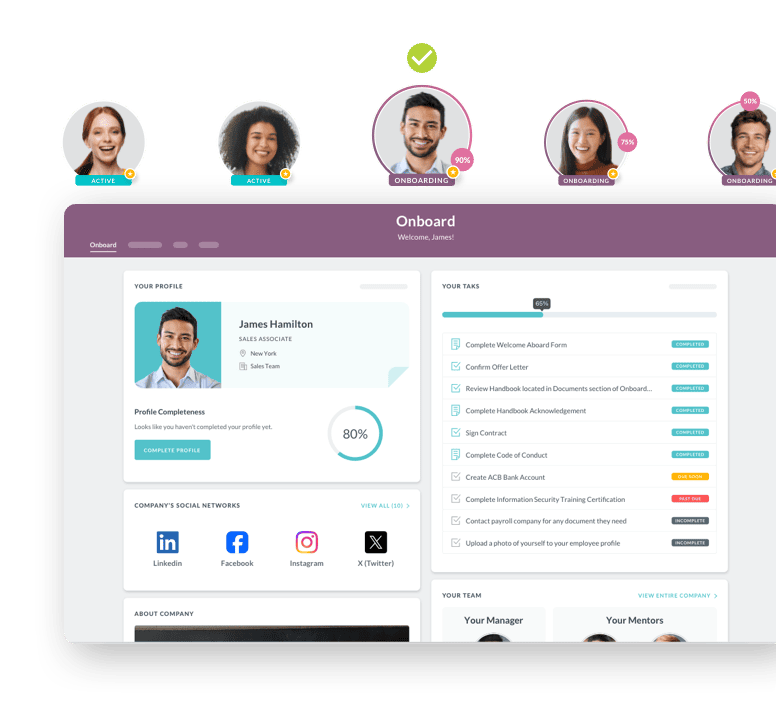
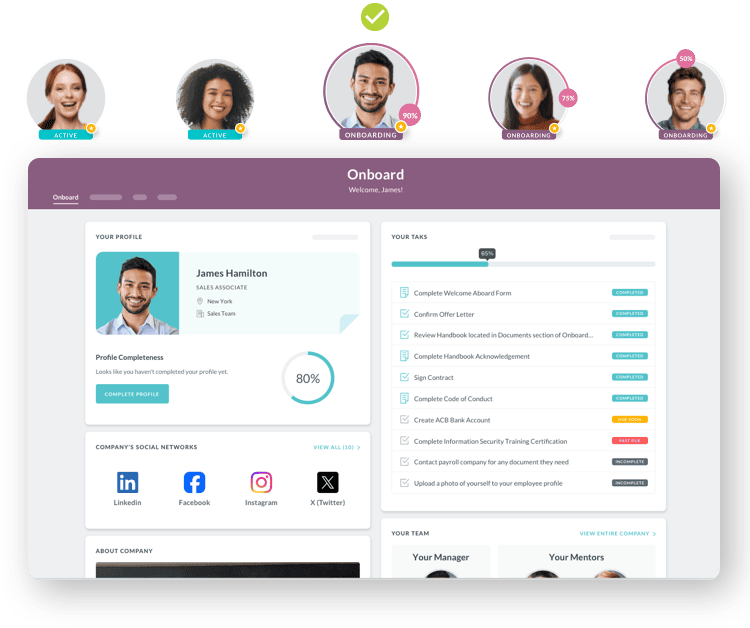
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Keep Reading
Why Healthcare Organizations Choose HR Cloud Over Alternatives
What is the Best Healthcare HR Software for Medical Organizations?
The Complete Guide to Remote Work Policy Compliance: Navigating Multi-State Tax, Legal, and Security Requirements in 2026
With 22.9% of US employees working remotely as of Q1 2024—up from 19.6% the previous year
Enterprise HRIS Implementation: Rippling vs HR Cloud Integration Capabilities and Deployment Success
Enterprise HR Software Implementation Comparison
Ready to streamline your onboarding process?
Book a demo today and see how HR Cloud can help you create an exceptional experience for your new employees.

