Is Spouse Losing Job a Qualifying Life Event?
- When Spouse Job Loss Qualifies as a Life Event
- Coverage Options During This Special Enrollment Period
- Best Practices for Managing Spousal Job Loss
- Pitfalls to Avoid During This Life Event
- Industry Applications of This Qualifying Event
- Implementation Plan for This Life Event
- Future Outlook and Trends
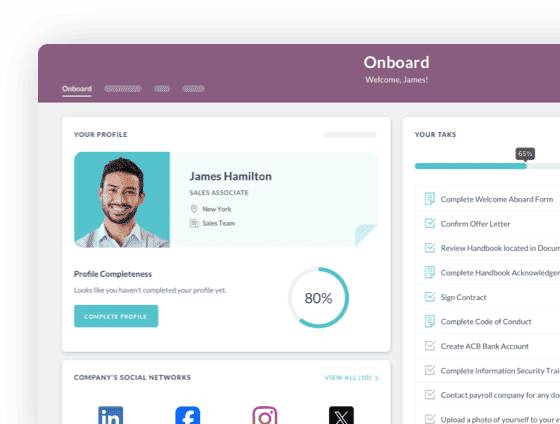
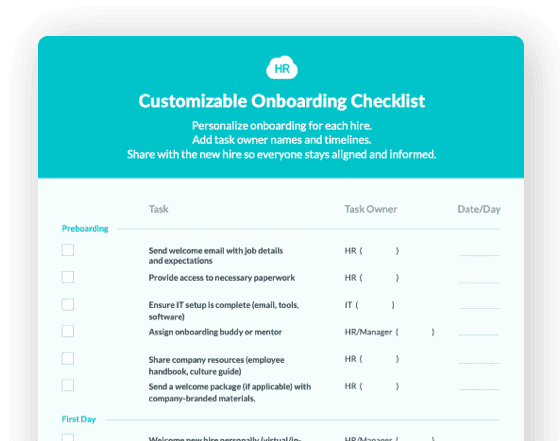
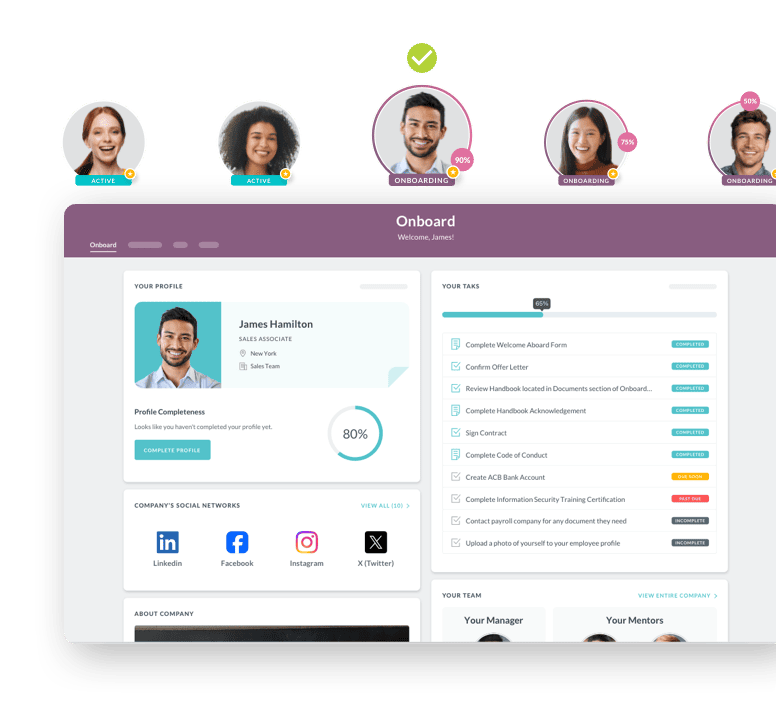
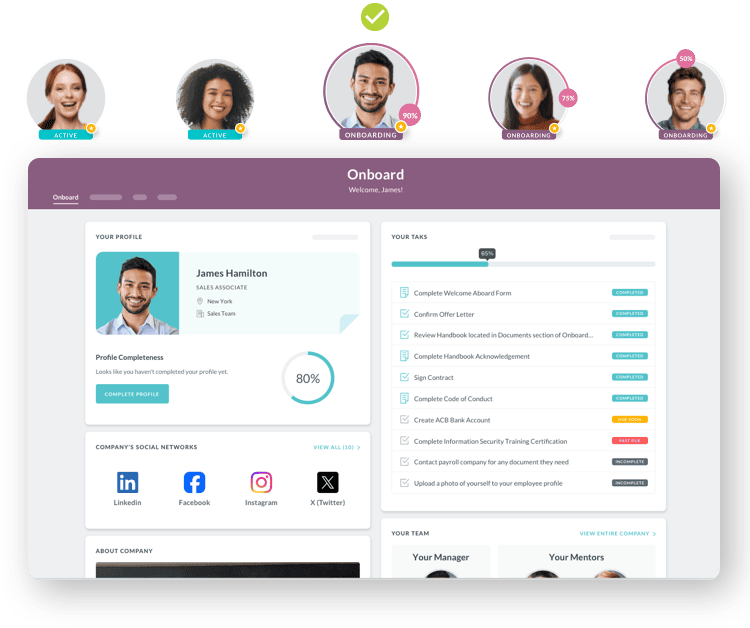
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
When your spouse loses their job, health insurance coverage becomes an immediate concern. The good news is that spousal job loss qualifies as a life event under federal law, allowing you to modify health benefits outside the normal enrollment period. This designation prevents costly coverage gaps during an already difficult transition.
A qualifying life event is a specific change in circumstances that permits you to adjust health insurance elections outside the annual open enrollment period. When your spouse loses their job and health coverage, you trigger a special enrollment period lasting 30 to 60 days. During this window, you can add your spouse to your employer's plan, explore marketplace options, or make other adjustments to ensure continuous protection.
This matters because most companies only allow benefits changes during brief enrollment windows. Missing your special enrollment period could force your family to wait months or pay expensive COBRA premiums. Understanding how this qualifying event works empowers you to act quickly and protect your family's health access when it matters most.
Why Spousal Job Loss Qualifies as a Life Event
Federal regulations recognize that losing employer-sponsored health insurance involuntarily should not force families into coverage gaps. When your spouse loses their job through layoffs, termination, resignation, or company closure, they typically lose health benefits within 30 days.
This creates what federal law calls a "change in status event." The reason for leaving doesn't matter. Voluntary resignations count the same as involuntary terminations. What matters is that qualifying coverage ended, protecting families regardless of circumstances.
-
The actual coverage loss date matters more than the employment end date
-
Only involuntary loss of coverage qualifies for special enrollment
-
The lost coverage must have been minimum essential coverage
-
You typically have 30 to 60 days to take action
-
Documentation requirements are strict and require official proof
-
The event affects all dependents covered under the lost plan
Coverage Options During This Special Enrollment Period
|
Coverage Option |
Typical Timeline |
Cost Consideration |
Key Advantage |
|
Spouse's Employer Plan |
30-60 day enrollment window |
Premium deducted from paycheck |
Immediate access to existing network |
|
Health Insurance Marketplace |
60 days from coverage loss |
May qualify for subsidies based on income |
Flexibility in plan selection |
|
COBRA Continuation |
Up to 18 months available |
Full premium plus 2% admin fee |
Maintains existing doctors and coverage |
|
Short-Term Plans |
Can start quickly |
Generally lower premiums |
Bridges gaps between major coverage |
This table helps you compare your primary options when responding to spousal job loss. Each pathway offers different benefits depending on your household's specific circumstances, income level, and healthcare needs. The right choice depends on factors including how quickly your spouse expects to find new employment, whether you have ongoing medical needs requiring specific providers, and what your current budget can accommodate during a period of reduced income.
Best Practices for Managing Spousal Job Loss
Quick action and organized documentation help you maximize coverage options while meeting strict deadlines.
Request written confirmation of coverage termination dates immediately. Contact your spouse's former HR department for official documentation showing exactly when coverage ends. This letter serves as proof for your special enrollment period and eliminates deadline confusion.
Notify your own HR department within a few business days. Most companies process benefits modifications within specific payroll cycles. Starting early allows time for complications or additional paperwork. Streamlined benefits administration systems make this smoother, but prompt action prevents delays.
Gather required documentation before submitting enrollment requests. According to SHRM guidance on benefits changes, having paperwork ready accelerates processing and prevents coverage gaps. You'll need termination letters, coverage end dates, marriage certificates, and dependent documentation.
Compare all available options thoroughly. Evaluate COBRA costs against employer plan premiums, marketplace subsidies, and timing for new coverage. COBRA allows continuation for up to 18 months but requires paying full premiums plus administrative fees, often costing more than alternatives.
Document everything in writing. Keep copies of all correspondence with HR departments and insurance carriers. Save email confirmations and enrollment receipts. Modern HRIS platforms create audit trails, but maintaining personal records adds security.
Pitfalls to Avoid During This Life Event
Common mistakes delay coverage or create unexpected protection gaps.
Missing enrollment deadlines entirely represents the most frequent error. The 30 to 60 day window seems generous until you factor in emotional stress, documentation logistics, and HR processing time. The countdown begins when coverage ends, not when you learn about job loss or start paperwork. This confusion causes families to miss their window entirely.
Failing to understand documentation requirements creates processing delays. Different companies have varying verification standards. Some require original letters on company letterhead while others accept electronic confirmations. Submitting inadequate proof pushes coverage start dates back weeks or causes complete missed enrollment periods. Healthcare organizations particularly maintain strict requirements due to compliance concerns.
Overlooking premium payment deadlines following enrollment represents another critical error. Making enrollment changes is only the first step. Missing payment dates means enrollment gets cancelled even after completing paperwork successfully.
Underestimating COBRA costs surprises many families. The full premium includes both employee and employer portions plus administrative fees. According to Healthcare.gov guidance, total costs often consume large portions of unemployment benefits.
Not exploring marketplace subsidies means potentially paying thousands more annually than necessary. If household income decreases, you might qualify for premium tax credits making marketplace coverage more affordable than employer plans during unemployment.
Industry Applications of This Qualifying Event
Spousal job loss impacts vary across sectors, influencing coverage decisions and alternative options.
Healthcare settings create complex situations because medical professionals have specialized coverage needs. A nurse whose spouse loses their pharmaceutical company job needs seamless coverage avoiding gaps that complicate professional credentialing. Many healthcare employers offer immediate enrollment or minimal waiting periods, recognizing that professionals prioritize continuity of care.
Technology sector employees face different dynamics. Tech companies provide generous benefits with low premiums, making spousal additions relatively affordable. However, high-income households won't qualify for marketplace subsidies, making thorough COBRA comparison essential for budget optimization during unemployment.
Manufacturing and construction industries present unique challenges because physical labor involves higher injury risks. Families may face immediate decisions about maintaining COBRA coverage for specialists treating work-related injuries versus switching to different networks. This becomes complex if job loss followed workplace injury requiring ongoing care from established providers.
Implementation Plan for This Life Event
Follow these steps to maintain continuous protection without delays.
Step 1: Confirm Coverage Termination Date
Contact your spouse's former HR department immediately to determine exactly when insurance ends. Request written confirmation establishing your timeline for all subsequent actions.
Step 2: Assess Your Employer's Benefits
Review your company's health insurance options within 48 hours. Contact HR to understand available plans, addition costs, waiting periods, and required documentation. Effective benefits administration makes this straightforward.
Step 3: Explore Marketplace Options
Visit Healthcare.gov to investigate available plans and subsidy eligibility based on current income. Research provides crucial comparison data about costs, coverage levels, and provider networks.
Step 4: Calculate COBRA Costs
Request COBRA premium information directly from your spouse's former HR department. Compare figures against other options, remembering COBRA maintains established provider relationships.
Step 5: Make Your Decision
Weigh monthly premiums, deductibles, out-of-pocket maximums, provider networks, and likelihood of securing new employment soon. For families with ongoing medical needs, COBRA might justify higher premiums despite costs.
Step 6: Submit Enrollment Paperwork
Complete required paperwork immediately once decided. Gather documentation including termination letters and marriage certificates. Submit through your employer's portal or marketplace, keeping submission copies.
Step 7: Follow Up on Status
Contact HR or your insurance provider three to five business days after submission to confirm receipt and processing. Proactive follow-up catches problems while time remains for corrections.
Step 8: Set Up Premium Payments
Ensure first premium payments process correctly and on time. For marketplace plans, pay the insurer directly. For employer plans, verify payroll deductions begin correctly to activate coverage.
Future Outlook and Trends
Benefits administration continues evolving as technology advances and workplace dynamics shift, reshaping how families navigate spousal job loss.
Artificial intelligence and automated benefits counseling tools are helping employees make better decisions during qualifying life events. These systems analyze circumstances, healthcare needs, and financial situations to recommend optimal coverage choices. As tools mature, they'll reduce anxiety and confusion during stressful transitions. Expect more companies adopting AI-powered platforms that guide employees through qualification, automatically verify documentation, and predict best coverage options based on historical patterns.
The rise of gig economy work and non-traditional employment will likely expand qualifying life event definitions. As more people move between contract work, freelancing, and traditional employment, the line between "employed with benefits" and "unemployed" continues blurring. This may pressure insurers and employers to develop more flexible enrollment policies accommodating fluid career paths.
Expect continued regulatory evolution around special enrollment periods. Recent years saw both expansions and contractions depending on political priorities. Staying informed through SHRM's benefits compliance resources ensures you understand rights and advocate effectively for coverage needs.
Employees increasingly demand more flexibility beyond traditional health insurance. Recognition that financial wellness, mental health support, and work-life balance contribute to overall wellbeing pushes companies toward diverse benefit portfolios. When spouses lose jobs, families face not just health insurance questions but concerns about retirement savings, childcare costs, and emergency resources. Forward-thinking employers respond with benefits ecosystems addressing these interconnected needs.
Understanding that spousal job loss qualifies as a life event provides critical foundation for protecting your family during uncertain times. Federal protections, employer policies, and marketplace options create multiple pathways to continuous coverage when you navigate the system effectively.
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Keep Reading
Key Elements of an Effective Manufacturing Onboarding Checklist: Complete Guide for HR Leaders
"Safety first isn't just a slogan—it's a survival strategy."
Top 9 Manufacturing Onboarding Software Features: Safety, Mobile-first, and More
Tell me the truth: that onboarding software your company has been using to onboard your
Manufacturing Employee Onboarding Software: Automate New Hire Training with Digital Workflows and Compliance Management
TL;DR: Manufacturing employee onboarding software reduces new hire time-to-productivity
Ready to streamline your onboarding process?
Book a demo today and see how HR Cloud can help you create an exceptional experience for your new employees.

