This blog identifies 10 common workforce management challenges hospitals and home care teams face—from scheduling complexity and credentialing bottlenecks to compliance risks and communication gaps—and offers practical solutions that fix them fast. It shows how purpose-built software and streamlined workflows can automate scheduling, track certifications, manage timekeeping, and reduce administrative load. Key takeaways include minimizing manual processes, improving shift visibility, and using real-time data for staffing decisions. The biggest value: actionable fixes that help healthcare HR teams boost operational efficiency, maintain compliance, and improve caregiver satisfaction without extra overhead.
10 Workforce Management Issues Hospitals and Home Care Teams Face (and What Fixes Them Fast)
.png)
- 1. Shift Scheduling Chaos That Cascades Across 24/7 Operations
- 2. Compliance Documentation That Disappears When Auditors Arrive
- 3. Time-Off Requests That Create Coverage Nightmares
- 4. Performance Reviews Perpetually Postponed Until "Things Slow Down"
- 5. Recognition Programs That Exist Exclusively in HR Policy Manuals
- 6. New Hire Onboarding That Overwhelms Rather Than Orients
- 7. Talent Leaving Because They Don't See Professional Growth Pathways
- 8. Payroll Errors That Systematically Erode Trust
- 9. Critical Data Scattered Across Incompatible Systems
- 10. Workforce Reporting That Requires Days to Generate
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
"We're hemorrhaging nurses faster than we can replace them, and our current systems can't even tell me which shifts are critically understaffed until it's too late."
That's what Dr. Rachel, Chief Nursing Officer at a 300-bed regional community hospital, told her executive team in November 2024. Her facility had just recorded its third consecutive quarter of nurse vacancy rates above 12%—well above the national average of 9.6%. The financial impact was staggering: $1.7 million in overtime costs, $420,000 in travel nurse contracts, and patient satisfaction scores declining alongside staff morale.
Dr. Rachel's situation wasn't unique, but the scale of what she faced was striking. Ten different workforce management challenges had tangled together, each one feeding the others. A scheduling conflict in one department would trigger a compliance gap somewhere else. The hospital had recognition programs—they were right there in the policy manual—but night shift staff had no idea they existed. Performance reviews were supposed to happen quarterly, and sometimes they actually did. Her affiliated home health division faced an entirely different set of problems across their 40-mile service territory, where caregiver shortages created a domino effect she couldn't seem to stop.
The healthcare workforce crisis has officially arrived. By 2028, the U.S. will face a shortage of 100,000 critical healthcare workers according to Health Resources & Services Administration projections. Over 50% of registered nurses currently practicing are above age 50, creating an impending retirement wave that will leave massive experience gaps precisely when demand intensifies. Home health agencies report that a single caregiver vacancy disrupts coverage across entire service territories, forcing existing staff into unsustainable schedules that accelerate turnover.
The financial mathematics are unforgiving. Healthcare organizations spent $1.7 billion on travel nurses in 2024. The average cost to replace a single registered nurse now exceeds $61,110 according to NSI National Healthcare Retention Report data, representing six to nine months of that position's salary consumed by recruitment, onboarding, and productivity ramp-up.
Here's what those workforce statistics don't tell you: these aren't separate problems that need separate solutions. They're all connected—symptoms of healthcare HR infrastructure that was never built to handle how complex medical delivery has become.
Understanding Hospital Workforce Management Software Requirements
If you're evaluating workforce management platforms, you need to know what actually makes a solution work for healthcare versus just another generic HR system with a medical logo slapped on it.
Hospital workforce management software has to juggle a lot at once: 24/7 shift scheduling, credential tracking across multiple locations, role-specific compliance workflows, staffing visibility, and integration with your existing payroll and clinical systems. Most conventional business HRIS platforms just weren't built for this.
|
Workforce Management Capability |
Manual/Spreadsheet Approach |
Generic Business HR Software |
Healthcare-Specific Platform (HR Cloud) |
|
24/7 Shift Scheduling |
Phone calls, spreadsheets, constant manual adjustments |
Basic calendar tools without shift-specific rules |
Automated scheduling with IP/geolocation restrictions for remote workers |
|
Compliance Documentation |
Paper files, scattered digital folders, manual expiration tracking |
Document storage without healthcare-specific workflows |
Automated I-9, E-Verify integration, license renewal alerts |
|
Performance Reviews |
Annual reviews often delayed, minimal peer input |
Generic review forms not customized for clinical roles |
Customizable cycles with peer/manager/self-review, competency tracking |
|
Time-Off Management |
Approval via email, no coverage visibility |
Basic PTO tracking without minimum staffing rules |
Policy-driven approvals with shift coverage conflict detection |
|
Multi-Location Coordination |
Separate systems per facility, no centralized reporting |
Limited multi-site functionality |
Unified platform with location-specific customization |
|
Implementation Timeline |
N/A |
12-18 months typical for enterprise systems |
Streamlined deployment designed for faster time-to-value |
1. Shift Scheduling Chaos That Cascades Across 24/7 Operations
Hospitals never close. Home care teams work scattered across service territories that can span dozens of zip codes. And the traditional ways of scheduling—spreadsheets shared via email, phone calls that turn into text message chains, handwritten assignment boards you have to physically walk over to see—they just fall apart when you try to scale them.
Here's how it breaks down. An ICU nurse ends up scheduled for back-to-back night shifts without the required 10-hour rest period between them. That violates facility policy and creates patient safety exposure. A home health aide doesn't get the updated visit schedule and shows up at the wrong patient's house 40 minutes away. Coverage gaps force clinical managers into those desperate last-minute phone calls, burning through goodwill and accelerating turnover among staff who are sick of unpredictable schedule changes.
You can see the cost in overtime line items and travel nurse contracts. But the hidden cost? Clinical managers spending 6-8 hours every week solving scheduling puzzles instead of supporting patient care. The American Hospital Association has drawn a direct line between inefficient scheduling and staff burnout—which matters when 49% of physicians are already reporting burnout symptoms, according to American Medical Association survey data.
Home Health Scheduling Platform Requirements
Home health organizations deal with scheduling complexity that hospitals don't have to think about. Your field staff work from patient homes, not a central facility. They need to hit precise appointment windows. Travel time between visits changes based on traffic, weather, and how spread out everything is. And when someone calls in sick, you can't just find any available replacement—you need someone who's actually close to those assigned patients.
"Scheduling fragility became a defining issue in 2025," according to Alora Health's industry analysis. "A single vacancy could disrupt coverage across an entire service area. Retention increasingly depended on realistic caseload expectations and predictable communication from leadership."
What resolves it: Centralized time and attendance management systems configured for role-specific requirements, shift preference accommodation, and automated compliance rule enforcement. HR Cloud's Time Clock uses geolocation restrictions to ensure employees clock in only from approved locations. This matters for home care workers who clock in from patient residences rather than central offices.
Clinical managers can approve timesheets across multiple locations, track hours with automatic updates, and identify coverage gaps before they escalate to operational emergencies. The system supports exceptional policies for specific roles, departments, or employment types. Organizations managing both hospital-based staff and distributed home care teams can use unified healthcare workforce management infrastructure.
2. Compliance Documentation That Disappears When Auditors Arrive
I-9 verification. Nursing license renewals you have to track across multiple state boards. Continuing education credits that expire on different schedules for everyone. Vaccination records—flu, hepatitis B, MMR, varicella, and now COVID-19 boosters. TB tests that need annual updates. Background checks with lookback periods that vary by state.
Healthcare compliance isn't something you can blow off. The penalties for documentation gaps are brutal. One lapsed nursing license creates immediate liability exposure and might violate state staffing ratio requirements. Missing I-9 documentation means substantial fines when Immigration and Customs Enforcement shows up. But when HR teams manage all this through scattered spreadsheets, shared drives, and actual physical file cabinets, critical renewal deadlines just slip through unnoticed until violations show up.
Home health agencies have it even worse. Field staff work remotely, which makes collecting documents in person a logistical nightmare. License requirements change from state to state—so if you're operating across state lines, you're tracking different credentialing requirements for the exact same job role. When an auditor requests documentation for 50 employees during an unannounced inspection, your team is frantically searching across multiple systems trying to find paperwork that's stored in who-knows-what format.
Healthcare HR Compliance System Capabilities
The National Council of State Boards of Nursing reports that approximately 4-6% of nursing licenses lapse annually due to missed renewal deadlines. For a 300-bed hospital employing 400 nurses, that represents 16-24 nurses potentially practicing with expired credentials—a compliance exposure many organizations don't discover until routine audits surface the violations.
What resolves it: Automated compliance workflows that trigger based on hire dates and role-specific requirements. HR Cloud's onboarding system includes built-in I-9 completion tasks with direct integration to E-Verify for electronic verification—eliminating manual paper-based processes vulnerable to errors and misplacement.
The platform auto-assigns compliance documents based on position, department, or location—ensuring home health aides in California receive different onboarding requirements than hospital nurses in New York, addressing state-specific regulatory variations automatically. Renewal reminder notifications prevent license lapses before they impact staffing availability. And when regulatory requirements change, centralized policy updates propagate across all affected employee records without manual intervention.
Michael, owner of a regional home health agency, explains their motivation for moving from paper processes to HR Cloud's onboarding platform: "We needed a better way to replace our manual, paper-based recruiting and onboarding systems. Onboard gave us confidence to place new hires in the field right away without worrying about compliance."
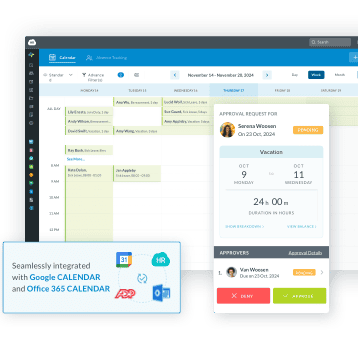
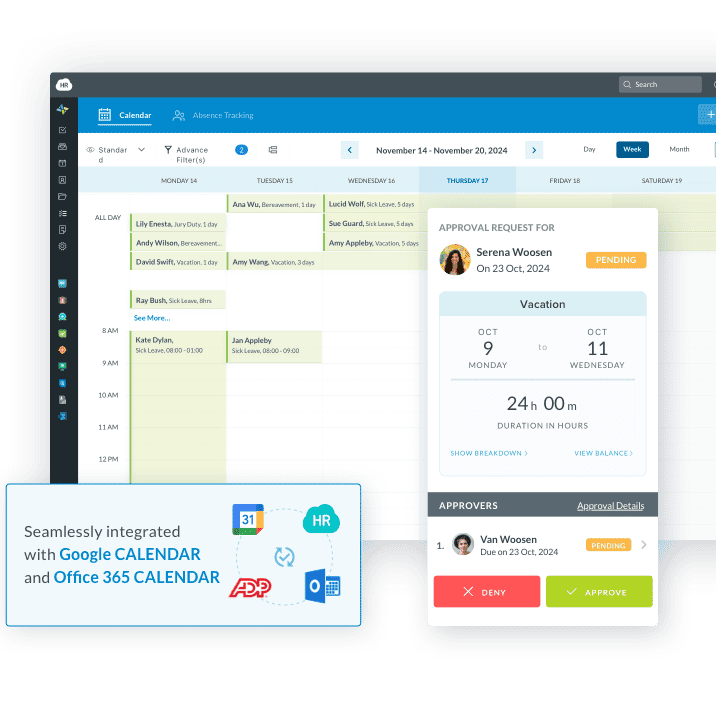
3. Time-Off Requests That Create Coverage Nightmares
A radiology technician requests three weeks off for emergency family care—starting in six days. Two emergency department nurses both put in requests for the same holiday weekend three months ago, and both got auto-approved without anyone checking departmental coverage. A home health coordinator forgets to factor in caregiver PTO when assigning patient visits, and now you've got missed appointments and frantic schedule reshuffling.
Time-off management in healthcare isn't just about tracking vacation balances. It's about maintaining minimum safe staffing ratios while still respecting actual employee needs. Manual approval processes create delays that frustrate staff. Managers approve requests without being able to see cross-shift coverage in their department, and they only discover conflicts when schedules get published. When conflicts show up and you have to deny requests, employees see inconsistency and favoritism—which breeds the kind of resentment that accelerates turnover.
The American Nurses Foundation identifies inadequate staffing and lack of schedule flexibility as top drivers of nurse turnover. When employees consistently experience time-off requests handled inconsistently or perceive approval processes as arbitrary, they begin exploring employment elsewhere. For organizations already facing 18.3% average hospital turnover rates (per NSI 2025 data), every preventable departure matters.
Comparison: Time-Off Management Approaches
|
Time-Off Management Feature |
Email-Based Approval |
Standalone Time-Off Software |
Integrated Healthcare HRIS (HR Cloud) |
|
Coverage Visibility |
None - manager approves without seeing team calendar |
Limited - shows who's off but not minimum staffing requirements |
Calendar view - shows who's scheduled off |
|
Policy Enforcement |
Manual - manager calculates accruals |
Automated accrual tracking |
Automated with healthcare-specific rules (shift differentials, tenure-based) |
|
Multi-Location Support |
Separate tracking per facility |
Basic multi-site |
Centralized with location-specific policy variations |
|
Mobile Access for Field Staff |
Email only |
Varies by vendor |
Native mobile app for home health workers |
What resolves it: Policy-driven time-off management with visibility into team calendars. HR Cloud's Time Off application supports multiple policy structures—accrued time-off with configurable schedules based on tenure, or up-front allocation at hire date or calendar year start.
Managers can view team calendars showing who's already scheduled off, helping identify potential conflicts before approving new requests. Auto-assignment rules ensure new hires receive appropriate policies based on role, department, or location without manual intervention. Calendar integration displays upcoming absences, enabling proactive scheduling adjustments before understaffing creates patient care risks.
The system tracks accruals automatically, handles carryover amounts when configured, and enforces maximum balance limits—removing calculation burden from managers while ensuring policy compliance. For home health organizations, field staff can submit requests from mobile devices and view approval status without waiting for email responses.
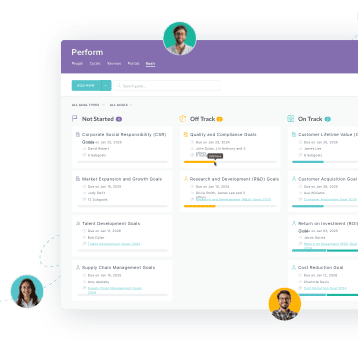
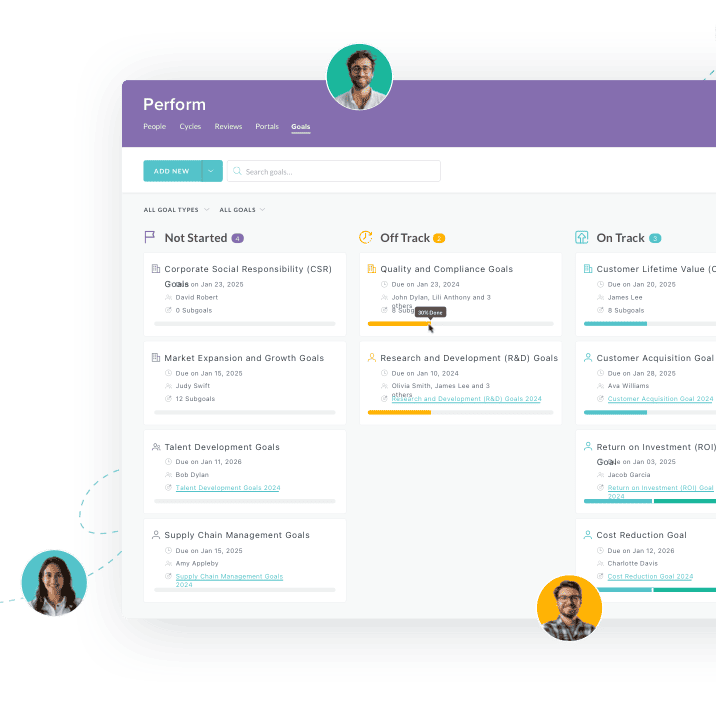
4. Performance Reviews Perpetually Postponed Until "Things Slow Down"
Performance management in healthcare follows a predictable pattern: HR mandates annual reviews. Clinical managers fully intend to complete them. Then patient care demands intervene. Reviews get pushed back weeks, then months. By the time evaluations actually happen, the feedback you're giving references situations from six months ago, and any chance for meaningful development conversations has basically evaporated.
Here's a stat: 96% of nursing homes report difficulty hiring qualified staff despite offering higher wages and sign-on bonuses, according to American Hospital Association data. Retention takes more than competitive pay. It requires ongoing feedback, visible development pathways, and consistent recognition that employees are actually progressing in their careers. But when performance management gets treated as administrative busywork instead of a strategic talent development tool, both managers and employees just check out completely.
The consequences stack up fast. High-potential clinical staff leave for organizations that actually invest in their professional growth. Struggling performers keep going without corrective feedback until problems reach the point where you need disciplinary action. Managers burn hours on last-minute documentation when HR sends those urgent reminders about overdue reviews approaching regulatory deadlines.
Performance Management in Healthcare Settings
Healthcare performance management differs from general business environments. Clinical roles require competency assessments tied to patient safety outcomes. Peer review processes integrate into medical staff credentialing. Performance data should correlate with quality metrics extracted from electronic medical records. And career progression often follows clinical ladder frameworks that generic review templates can't accommodate.
"Performance management for clinical roles requires competency assessments, quality metrics integration from EMR systems, patient satisfaction correlation analysis, and clinical ladder progression tracking," according to analysis from HR Cloud's healthcare software research.
What resolves it: Structured performance cycles with automated workflows and stakeholder notifications. HR Cloud's Perform application enables customizable review cycles—annual, quarterly, or triggered by specific milestones like probationary period completion or role changes.
The system supports self-review, manager review, peer review, and direct report review configurations—critical for clinical environments where peer evaluation provides insights managers can't observe directly. Administrators assign reviews based on department, location, position, or custom criteria. The platform tracks completion status, sends automated reminders escalating to supervisors, and generates cross-team performance reports and analytics.
These analytics help identify both top performers worthy of retention investment and struggling employees requiring additional support before performance issues escalate. Organizations can configure overall rating scales, set visibility permissions controlling who sees completed reviews, and enable goal tracking to connect performance conversations to strategic objectives.
According to the system's capabilities, administrators can assign performance reviews to employees who weren't part of the original criteria by manually selecting individuals and choosing "Assign Performance Review" from the Actions menu—useful when organizational changes require adding employees mid-cycle.
5. Recognition Programs That Exist Exclusively in HR Policy Manuals
Every hospital says they're committed to recognizing employee contributions. Most home health agencies put recognition language in their recruitment materials. But when actually giving that acknowledgment requires manager initiative, multi-step approval workflows, and filling out forms during nonexistent administrative time, recognition happens sporadically if it happens at all—and it never reaches night shift workers who rarely cross paths with daytime leadership.
Frontline healthcare workers need timely, specific recognition. Nurses managing unstable patients. Aides providing personal care. Therapists rehabilitating stroke survivors. Environmental services staff maintaining sterile environments. They don't need annual awards ceremonies with predictable winners or generic "employee of the month" programs that everyone cynically views as political. They need real-time acknowledgment when they exceed expectations or demonstrate organizational values under pressure.
Research consistently shows the link between meaningful recognition and both engagement and retention. Organizations with effective recognition programs see 31% lower voluntary turnover, according to Gallup workplace research. But healthcare organizations struggle to implement recognition systems that feel authentic and accessible to staff working nights, weekends, and remote schedules far from central administration.
Employee Recognition Software for Healthcare Organizations
Recognition in healthcare environments requires mobile-accessible platforms that function across distributed workforces. It needs to integrate with existing communication tools that clinical staff already use. And it should support both peer-to-peer recognition and manager acknowledgment, since direct observation opportunities vary dramatically by role and shift.
What resolves it: Peer-to-peer recognition platforms integrated into daily workflows rather than requiring separate logins. HR Cloud's Kudos feature within the Workmates application enables employees and managers to give instant recognition tied to company values through a mobile interface.
Organizations can configure point-based reward systems where Kudos recipients accumulate points redeemable for gift cards or custom rewards like additional PTO, preferred parking, or schedule flexibility. The platform supports spending limits controlling how many points users can distribute within specified periods, preventing point inflation while encouraging consistent recognition.
The system helps identify employees who consistently deliver exceptional service warranting retention investment, and creates visible culture of appreciation that doesn't require manager gatekeeping. Recognition appears in feeds visible to the organization, amplifying impact beyond private thank-you messages.
A talent development manager at a multi-state organization with 3,400+ employees describes their experience implementing Workmates: "We highly recommend Workmates as it gives us the ability to communicate and connect our workforce." That same pattern applies to multi-site healthcare providers using targeted communications and recognition to reduce turnover.
6. New Hire Onboarding That Overwhelms Rather Than Orients
A newly hired home health nurse gets a 47-page policy manual via email attachment, three compliance forms with unclear instructions, and a list of patient home addresses with zero context about case complexity or visit priorities. Her official start date is Monday. The forms are due Friday. She won't get electronic access to scheduling systems and electronic medical records until her third day. She's already second-guessing her decision to take this job.
Healthcare onboarding carries a level of complexity that makes poor execution really costly. Clinical staff need role-specific training on equipment operation, emergency protocols, and facility-specific policies. The compliance documentation goes way beyond generic business requirements—I-9 verification, background checks, drug screening, health clearances, immunization records, license verification, malpractice insurance, HIPAA training, OSHA safety modules, and patient privacy acknowledgments.
When new hires feel overwhelmed or unsupported during those first few weeks, they're way more likely to resign during probationary periods. That's expensive when you consider that replacing a single RN costs over $60,000 including recruitment, onboarding, and productivity ramp-up, according to NSI data. Early turnover also damages team morale because existing staff have to absorb extra work while positions sit vacant pending new replacement cycles.
Healthcare Onboarding Software Requirements
The problem gets worse with remote workers. Home health aides don't have a physical office to visit for in-person orientation. They work independently from day one, often covering massive geographic territories. When your onboarding relies on email attachments and phone calls, critical steps get missed—and you only discover those compliance gaps when regulatory audits roll around.
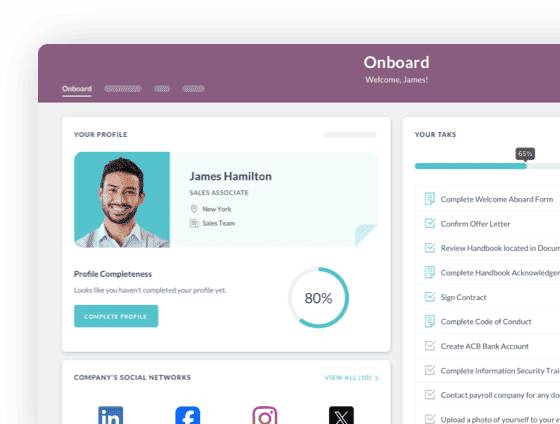
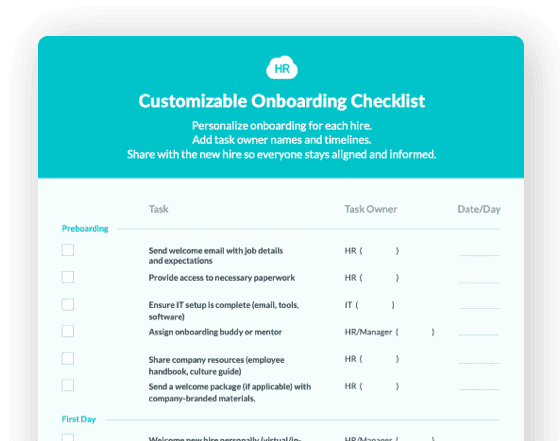
What resolves it: Structured onboarding checklists with role-based task assignment and progress tracking. HR Cloud's Onboard application enables organizations to create position-specific checklists that trigger automatically based on hire date or employment status changes.
Tasks can be assigned to new hires, managers, HR administrators, IT staff, or facilities personnel—with due dates, automated notifications, and completion tracking visible to stakeholders. For home health agencies, the system supports remote document completion and digital signature collection, eliminating need for new hires to travel to central offices for paperwork sessions.
New hires complete I-9 verification, direct deposit enrollment, and policy acknowledgments from any device. HR teams monitor onboarding completion across all new hires through centralized dashboards, identifying bottlenecks before they cause start date delays or compliance gaps.
A behavioral health provider experienced a 60% reduction in procedural queries from new hires after implementing streamlined onboarding with clear digital checklists. Their onboarding timeline compressed from 4 weeks to 2.5 weeks, allowing clinical staff to contribute sooner while reducing administrative overhead.
 — Travis French, CEO, Renaissance Outpatient Rehabilitation Center
— Travis French, CEO, Renaissance Outpatient Rehabilitation Center 

7. Talent Leaving Because They Don't See Professional Growth Pathways
Healthcare confronts a retention paradox. Organizations desperately need experienced clinical staff. Nursing vacancy rates average 9.4% nationally, with some specialties experiencing shortages above 15%. Yet many hospitals and home health agencies lack formalized career development programs that help employees visualize advancement opportunities beyond lateral moves to competing employers.
A talented medical assistant wants to become a registered nurse but doesn't know if her employer offers tuition assistance or maintains partnerships with nursing schools. A home health aide interested in pursuing LPN licensure doesn't see examples of others who've successfully made that transition within the organization. An ICU nurse with leadership potential doesn't receive mentoring, management training, or visibility into nurse manager career progression.
When employees don't see growth opportunities, they accept offers from organizations that demonstrate investment in development. Healthcare can't afford losing people who've already proven clinical competence, cultural fit, and institutional knowledge. The Association of American Medical Colleges projects physician shortages approaching 86,000 by 2036—making retention of existing talent increasingly critical as pipeline constraints limit replacement capacity.
Career Development in Healthcare Settings
Employee development in healthcare extends beyond generic professional development. It includes clinical ladder progression, specialty certifications, continuing education requirements, preceptor training, leadership development for charge nurse roles, and pathways from entry-level positions (CNA, medical assistant) to licensed roles (LPN, RN, advanced practice).
What resolves it: Performance management systems that include goal-tracking and development planning as integrated components. HR Cloud's Perform application enables goal assignment as part of performance cycles, creating documented development plans tied to organizational objectives and individual aspirations.
Managers and employees collaboratively set goals related to skill acquisition, certification completion, or leadership development during review conversations. Progress tracking provides accountability and visibility. When performance reviews include forward-looking development discussions—not just backward-looking evaluations—employees see tangible evidence that the organization invests in their long-term success rather than treating them as interchangeable labor resources.
The system supports goal templates that can be customized by role or department, ensuring clinical development goals align with competency frameworks and specialty requirements. Administrators can generate reports showing goal completion rates across departments, identifying areas where development support requires strengthening.
8. Payroll Errors That Systematically Erode Trust
A home health aide worked 52 hours last week including weekend visits, but her paycheck reflects only 40 hours at base pay. A hospital nurse's night shift differential wasn't applied correctly to three consecutive pay periods. An overtime calculation missed hours from a weekend shift that started Saturday night and extended past midnight into Sunday morning, affecting both shift differential and overtime rate calculations.
Payroll errors in healthcare carry amplified damage compared to industries with standard 9-to-5 schedules. Clinical staff work complex schedules across multiple shifts, often with differential pay for nights, weekends, holidays, on-call hours, and overtime. When errors occur—and when employees must chase down corrections through multiple follow-up conversations—trust erodes rapidly.
The problem compounds when time tracking and payroll systems don't communicate effectively. Data gets manually re-entered between platforms, introducing transcription errors. Managers approve timesheets in one system while payroll processes in another, creating reconciliation challenges. When discrepancies surface—often discovered only when employees review paychecks and question amounts—investigating them requires reconstructing data from multiple sources and identifying where the breakdown occurred.
Healthcare Payroll Integration Requirements
For home health organizations, payroll complexity intensifies. Field staff work across multiple patient locations. They may have mileage reimbursements tied to visit schedules. Travel time between appointments may or may not count as compensable hours depending on state regulations. And when workers cross state lines serving patients in border regions, multi-state tax withholding requirements create additional compliance exposure.
What resolves it: Integrated time tracking and payroll system connections that reduce manual data transfer. HR Cloud offers direct integrations with major payroll platforms including ADP Workforce Now, ADP TotalSource, Paylocity, and Dayforce.
Managers review and approve timesheets within HR Cloud, with approved hours ready for payroll processing. The integration reduces manual entry errors and eliminates redundant data entry across systems.
The integration supports complex healthcare pay scenarios including shift differentials, overtime calculations for FLSA-exempt and non-exempt employees, multi-location tracking with different pay rates, and on-call hours. For home health workers, geolocation tracking provides auditable records of time spent at patient locations—critical documentation for reimbursement verification and labor law compliance.
9. Critical Data Scattered Across Incompatible Systems
HR manages employee records in one vendor's platform purchased five years ago. Scheduling happens in Excel spreadsheets emailed weekly to department managers. Compliance documents live in physical file cabinets supplemented by scanned PDFs in shared drives with inconsistent naming conventions. Performance reviews are stored as Word documents attached to email threads. Time tracking uses a separate point solution that doesn't integrate with payroll. Credentialing for medical staff operates through specialty software that doesn't connect to core HRIS.
This fragmentation creates cascading operational problems. Reporting requires manually pulling data from disparate sources and reconciling conflicting information. Simple questions—"How many employees are due for license renewal this quarter?" or "What's our average time-to-hire by department?"—demand hours of compilation work. Onboarding new technology requires integrating with multiple existing systems, each with different data formats and API capabilities.
For multi-location healthcare organizations, fragmentation intensifies exponentially. Hospital divisions use different systems than home health divisions. Regional variations in regulatory requirements complicate standardization efforts. When leadership requests enterprise-wide workforce analytics—comparing turnover rates across facilities, analyzing time-off patterns by location, or identifying high-performers based on recognition data and performance scores—producing accurate reports becomes a major project requiring dedicated analyst resources.
Healthcare HRIS Platform Architecture
The average healthcare organization uses 16 different software systems for workforce management according to HIMSS analytics. Each system requires separate logins, training, vendor management, and integration maintenance. IT departments spend substantial resources managing interfaces between platforms that should communicate seamlessly. And when data conflicts emerge—the same employee showing different hire dates in different systems—resolving discrepancies consumes HR staff time.
What resolves it: Unified HR platforms that consolidate core workforce management functions into integrated environments. HR Cloud combines employee records, time tracking, performance management, onboarding, compliance documentation, and recognition into a single platform with unified data architecture.
Employees access everything through one interface with single sign-on. Managers don't toggle between systems to approve time-off requests, review timesheets, and conduct performance evaluations—all functions operate within the same platform. HR teams generate cross-functional reports comparing turnover rates across departments, analyzing time-off patterns by location, or identifying high-performers based on combined recognition data and performance scores.
The platform supports role-based permissions configurable by position, ensuring clinical managers see relevant workforce data without accessing sensitive HR information like salary details or disciplinary records. For organizations managing both hospital and home health operations, the system accommodates location-specific policy variations while maintaining centralized visibility for executive reporting.
An outpatient care facility saved the equivalent of two full-time HR positions by automating onboarding, compliance tracking, and training workflows after consolidating onto a unified platform—freeing HR staff to focus on strategic initiatives rather than administrative data reconciliation.
10. Workforce Reporting That Requires Days to Generate
A hospital CFO requests workforce cost data broken down by department and compared year-over-year. An HR director needs turnover analytics comparing this year to last year, segmented by role, tenure, and reason for departure. A home health administrator wants real-time visibility into which caregivers are approaching overtime thresholds before the pay period closes, enabling proactive schedule adjustments.
These requests represent reasonable business intelligence needs. Yet when data lives in multiple systems and reporting requires manual compilation, producing these analyses consumes days of staff time. And by the time reports are finalized—often a week or more after the initial request—the opportunity to take preventive action may have already passed.
Healthcare organizations need real-time visibility into workforce metrics that inform operational decisions. Not monthly reports describing what already happened. Not manual queries requiring IT department involvement and multi-day turnaround times. Accessible dashboards showing current staffing levels, upcoming compliance deadlines, emerging turnover patterns, and cost trends that enable proactive management rather than reactive crisis response.
Healthcare Workforce Analytics and Reporting
Effective workforce analytics in healthcare must accommodate complexity that generic business intelligence tools don't address. Clinical roles have specialty-specific credentialing requirements. Shift schedules operate 24/7 with weekend and holiday variations. Patient census fluctuations create variable staffing needs. And regulatory reporting requirements demand specific data formats for Joint Commission, CMS, and state health departments.
What resolves it: Built-in analytics and customizable reporting integrated across all workforce functions. HR Cloud's Perform application includes matrix reports displaying performance scores and potential ratings across employees, with filtering by department, location, position, or employment type—enabling identification of high-performers and development needs at a glance.
The Time Clock module tracks hours across pay periods with customizable views showing regular hours, overtime, and shift differential breakdowns by employee or department. Time Off analytics display accrual balances and upcoming absences, enabling proactive coverage planning before shortages create patient care risks.
Because all data resides in a unified system with consistent data architecture, administrators create custom reports combining data points across functions. For example, correlating recognition frequency with turnover rates to determine whether departments with robust recognition cultures experience better retention. Or analyzing whether employees who complete scheduled performance reviews show different tenure patterns than those whose reviews are perpetually delayed.
These analytics enable workforce strategy refinement based on evidence rather than assumptions, helping healthcare leaders understand which retention initiatives generate measurable ROI and which programs consume resources without corresponding impact.


The Real Problem: Fragmented Systems, Not Missing Technology
Dr. Rachel's hospital didn't have a scheduling problem or a recognition problem or a compliance problem in isolation. It had a systems architecture problem. Disconnected processes made every workforce challenge exponentially harder to resolve than necessary.
By April 2025, her leadership team had implemented an integrated workforce management platform purpose-built for healthcare operations. Scheduling became data-driven with visibility into coverage gaps rather than reactive crisis management. Compliance documentation shifted from manual expiration tracking to automated renewal workflows with proactive alerting. Performance reviews happened on schedule with standardized peer and manager input rather than sporadic delayed conversations. Recognition became visible and immediate through mobile-accessible platforms. New hire onboarding followed structured checklists reducing time-to-productivity rather than ad hoc email chains creating confusion.
Did the nursing shortage disappear? No. Healthcare faces structural workforce constraints that technology alone won't resolve. But measurable improvements emerged within six months that justified the platform investment:
-
Nurse vacancy rates declined from 12.1% to 8.7%—still elevated but approaching manageable levels
-
Overtime costs decreased 22% year-over-year as scheduling visibility improved
-
Time spent on administrative workforce tasks fell 31%, freeing clinical managers for patient care support
-
Employee satisfaction scores measured through engagement surveys showed statistically significant improvement
-
Compliance audit findings dropped from 14 documentation gaps to 2 minor issues requiring remediation
These operational improvements translated to quantifiable financial impact. Using NSI's calculation that each percentage point reduction in RN turnover saves approximately $289,000 annually for an average hospital, the facility's 3.4 percentage point improvement in nurse retention represented nearly $1 million in avoided turnover costs—effectively funding the platform investment through retention gains alone.
Healthcare Workforce Management Software: Strategic Implementation Considerations
Organizations evaluating hospital workforce management software or home health scheduling platforms should assess solutions across multiple dimensions beyond initial feature checklists:
Integration Architecture: Does the platform integrate with existing payroll systems (ADP, Paylocity, Dayforce), background check providers (Checkr), and communication tools (Microsoft Teams, Slack)? Can it exchange data with electronic medical records and hospital management systems? Integration quality determines whether implementation adds to your technology stack complexity or simplifies it.
Mobile Functionality: What percentage of your workforce works outside traditional office environments? Home health workers, night shift nurses, and environmental services staff need full platform functionality from mobile devices—not just limited "view only" access. Mobile-first design ensures adoption across distributed workforces.
Compliance Capabilities: Does the system handle I-9 verification with E-Verify integration? Can it track role-specific licenses and certifications with automated renewal alerts? Does it accommodate multi-state regulatory variations for organizations operating across state lines? Healthcare compliance requirements exceed general business needs substantially.
Scalability and Multi-Location Support: Can the platform handle organizational growth from 50 to 500 to 5,000 employees without performance degradation? Does it support location-specific policy customization while maintaining centralized reporting visibility? Multi-facility healthcare systems require platforms architected for distributed operations.
Implementation Timeline: What's the realistic deployment schedule? Enterprise healthcare HR software alternatives typically require 12-18 months for full implementation. Purpose-built healthcare HRIS platforms often achieve faster time-to-value through streamlined configuration processes designed for medical environment complexity.
Vendor Healthcare Expertise: Does the vendor understand healthcare workforce management nuances—shift differentials, credentialing workflows, clinical ladder frameworks, Joint Commission requirements? Generic HR software vendors typically require extensive customization to accommodate healthcare-specific needs, while platforms purpose-built for medical environments offer healthcare functionality out of the box.
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Conclusion: The Healthcare Organizations That Thrive in Tight Labor Markets
The healthcare workforce crisis is real. The shortage projections from HRSA and AAMC are sobering. By 2037, physician shortages may reach 86,000. Nursing shortfalls will impact both hospital and long-term care settings. Home health demand is growing faster than workforce supply as aging demographics increase need for in-home services.
But organizations that modernize their workforce management infrastructure create competitive advantages in recruiting and retaining talent despite broader market constraints. When administrative processes work efficiently, clinical staff spend less time navigating bureaucratic friction and more time on work they trained for. When recognition happens consistently, employees feel valued. When career development is visible and supported through structured performance management, talented people stay.
The healthcare facilities that thrive in tight labor markets aren't necessarily those with the largest budgets for sign-on bonuses and premium compensation packages. They're the organizations that make working there less painful through better systems, clearer processes, and integrated tools that respect employees' time and intelligence.
Healthcare workers didn't enter the profession to wrestle with scheduling conflicts, chase down missing compliance documents, or wonder whether their contributions get noticed. They came to care for patients. Workforce management systems should support that mission—not obstruct it.
Schedule a demo to see how integrated HR solutions address workforce management challenges across hospitals and home health operations.
Related Resources:

Keep Reading
Caregiver Turnover in Home-Based Care: 5 Fixes That Actually Work
Home healthcare agencies face alarming turnover rates of 75%, with most caregivers
10 Workforce Management Issues Hospitals and Home Care Teams Face (and What Fixes Them Fast)
"We're hemorrhaging nurses faster than we can replace them, and our current systems can't
Key Elements of an Effective Manufacturing Onboarding Checklist
Manufacturing onboarding requires specialized checklists addressing safety compliance,
Like What You Hear?
We'd love to chat with you more about how HR Cloud® can support your business's HR needs. Book Your Free Demo

Build a Culture of Recognition. Boost Engagement. Guaranteed.
Workmates empowers employees to stay informed, connected, and appreciated—whether they’re on the front line, in the office, or remote. Recognition drives 12x higher engagement.Trusted by industry leaders in every sector




Cut Onboarding Costs by 60%.
Take the confusion and follow-ups out of onboarding with automated workflows, digital forms, and structured portals—so new hires ramp faster 3X quicker.Trusted by industry leaders in every sector