Primary and Secondary Insurance
- Understanding Primary and Secondary Insurance Coverage
- Key Points: How Primary and Secondary Insurance Work
- Primary vs Secondary Insurance: Side-by-Side Comparison
- Best Practices for Managing Dual Insurance Coverage
- Pitfalls to Avoid with Dual Insurance Coverage
- Industry Applications: Dual Coverage in Different Sectors
- Implementation Plan: Setting Up Effective Dual Coverage Management
- Future Outlook and Trends: Evolving Insurance Coordination
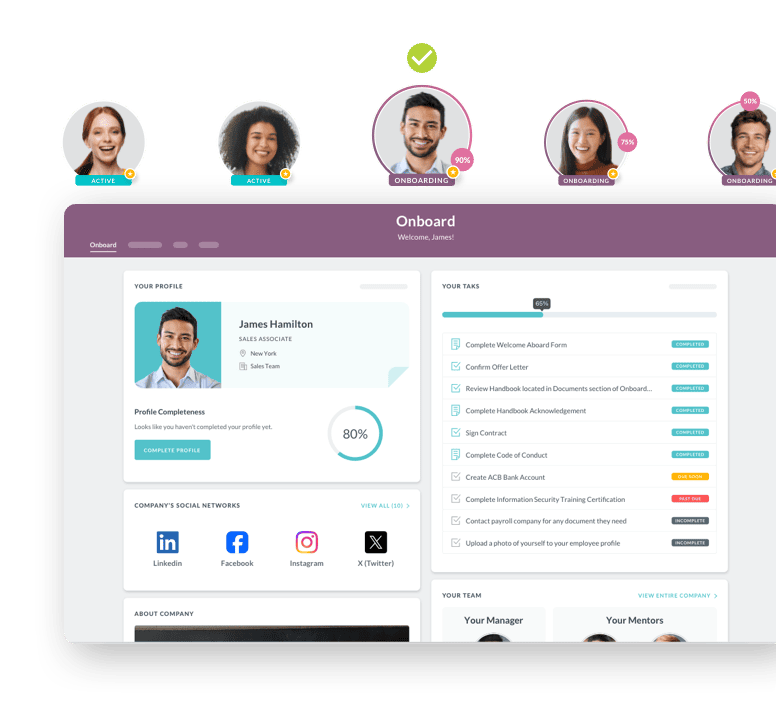
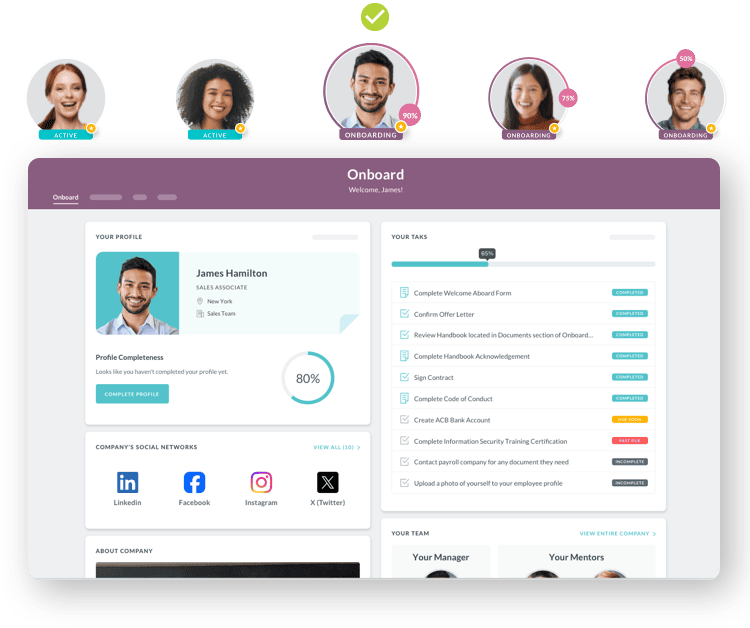
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
When employees have more than one health insurance plan, understanding which plan pays first can prevent confusion and unexpected medical bills. Primary and secondary insurance work together through a process called coordination of benefits. Your primary insurance pays first when you receive medical care. Your secondary insurance then covers some or all of the remaining costs. This system helps employees maximize their coverage while preventing duplicate payments. Business leaders who understand how these plans interact can better guide their teams through benefits decisions and reduce administrative headaches.
Understanding Primary and Secondary Insurance Coverage
Primary insurance is your main health plan. It processes medical claims first and pays benefits according to its coverage terms. This is typically the insurance you receive through your employer, or if you work for yourself, the plan you purchased directly. The primary plan does not know or care if you have other insurance. It simply pays what it would normally pay based on your policy.
Secondary insurance kicks in after your primary plan has paid its share. According to guidance from Medicare, the secondary payer only covers costs if the primary insurance did not pay everything. This might include your deductible, copayments, or coinsurance amounts. The secondary plan reviews what the primary plan paid and then determines if it will cover any remaining eligible expenses.
This coordination matters for businesses because employees with dual coverage need clear guidance during benefits administration. When your HR team understands how these plans work together, they can help employees make smarter choices during open enrollment and avoid billing problems that create frustration and lost productivity.
Key Points: How Primary and Secondary Insurance Work
These fundamental concepts help you understand how dual coverage operates in practice:
-
The primary plan always pays first, regardless of which plan offers better coverage. You cannot choose to submit claims to your secondary insurance first, even if it has lower copays or deductibles. The coordination of benefits rules determine payment order automatically.
-
Secondary insurance does not double your coverage or reimburse you twice. The Centers for Medicare and Medicaid Services ensures that combined payments never exceed 100% of the actual medical costs. This prevents overpayment while maximizing your coverage.
-
The birthday rule determines primary coverage for children when both parents have insurance. The parent whose birthday comes earlier in the calendar year provides the primary coverage. This standard rule eliminates confusion for families with dual coverage.
-
Employment status affects which plan is primary when Medicare is involved. If you work for an employer with 20 or more employees, your group health plan pays first. If your employer has fewer than 20 employees, Medicare becomes the primary payer.
-
COBRA coverage always serves as secondary insurance when you have other coverage. This matters when employees leave your company but maintain COBRA while covered under a spouse's plan.
-
Your HRIS platform should track coordination of benefits information to support accurate payroll deductions and benefits management. This prevents employees from paying premiums for duplicate coverage they do not need.
Primary vs Secondary Insurance: Side-by-Side Comparison
|
Feature |
Primary Insurance |
Secondary Insurance |
|
Payment Order |
Processes and pays claims first |
Pays remaining costs after primary |
|
Coverage Amount |
Pays full benefit according to policy |
Covers eligible costs up to 100% total |
|
Common Sources |
Employer plan, Medicare (age 65+) |
Spouse's plan, Medicare Supplement |
|
Claim Submission |
Provider bills this insurance first |
Billed after primary EOB is received |
|
Premium Cost |
Usually the main insurance expense |
Additional cost for extra protection |
|
Decision Control |
COB rules determine automatically |
Cannot choose to make this primary |
Best Practices for Managing Dual Insurance Coverage
Smart benefits management requires clear processes and employee education. These practices help your organization handle dual coverage effectively:
Collect complete insurance information during employee onboarding. Your new hire paperwork should ask about all insurance coverage, including spouse plans, Medicare, COBRA, and military benefits. This information prevents billing delays and claim denials. Train your HR team to update this information annually during open enrollment and whenever life events occur.
Educate employees about coordination of benefits rules. Many workers assume they can choose which insurance to use first or believe secondary insurance will eliminate all out-of-pocket costs. Neither assumption is correct. Create simple, clear materials explaining how dual coverage works. Include real examples showing how claims flow from primary to secondary insurance.
Verify coverage details before employees enroll in secondary plans. Sometimes the additional premium cost exceeds the actual benefit received. Help employees calculate whether secondary coverage makes financial sense based on their health needs and existing benefits. Your benefits administration system should provide tools for these comparisons.
Establish clear procedures for handling coordination of benefits questions. Employees will need help determining which plan is primary, especially in complex situations involving Medicare, COBRA, or divorced parents covering children. Create a reference guide your HR team can use to answer common questions quickly and accurately.
Document everything related to dual coverage decisions. Keep records of which employees have secondary coverage, what type it is, and when they enrolled. This documentation protects your organization if disputes arise about coverage or premium deductions. It also helps during HR compliance audits.
Pitfalls to Avoid with Dual Insurance Coverage
Even experienced HR professionals make mistakes with coordination of benefits. Understanding these common errors helps you avoid costly problems:
Assuming employees understand how secondary insurance works creates unnecessary confusion. Most people think secondary insurance means double coverage or that they can choose which plan to use first. Neither is true. Without clear education, employees make poor enrollment decisions and feel frustrated when bills do not get paid as expected. Provide written materials and hold benefit fairs where employees can ask questions.
Failing to update insurance information when life events occur leads to claim denials. Marriages, divorces, job changes, and Medicare enrollment all affect coordination of benefits. Set up automatic reminders for employees to update their information when these events happen. Make the update process simple through your employee self-service portal.
Overlooking Medicare coordination rules causes serious billing problems. When employees turn 65 or become Medicare-eligible due to disability, the coordination of benefits rules change dramatically. Employer size determines whether group insurance or Medicare pays first. Missing this distinction creates claim rejections and angry employees who thought their coverage was handled correctly.
Allowing employees to drop primary coverage while keeping secondary coverage wastes money. Some workers want to drop their employer insurance and keep only their spouse's plan because the spouse's coverage costs less. However, if your employer plan was primary, dropping it makes the spouse's plan primary and eliminates the coordination benefit. Employees end up paying more out of pocket than they saved in premiums.
Ignoring state-specific coordination rules creates compliance headaches. While federal coordination of benefits guidelines exist, some states have additional requirements. Make sure your benefits team knows the rules in every state where you have employees. This becomes critical for remote workers who might live in different states than your headquarters.
Industry Applications: Dual Coverage in Different Sectors
Coordination of benefits affects industries differently based on workforce characteristics. Here is how various sectors handle dual coverage:
Healthcare organizations face unique challenges because many employees become eligible for Medicare while still working. Nurses, physicians, and other clinical staff often continue working past age 65. These employers must carefully manage the transition between employer coverage as primary and Medicare as primary. Healthcare HR teams need specialized knowledge about Medicare Secondary Payer rules and must educate employees about enrollment timing to avoid gaps in coverage or late enrollment penalties.
Manufacturing companies with strong union representation often provide retiree health benefits. When retirees turn 65 and become Medicare-eligible, coordination between retiree coverage and Medicare becomes complex. Smart manufacturers provide dedicated counseling sessions to help retiring employees understand how their company coverage coordinates with Medicare. This reduces confusion and demonstrates the company values its retirees beyond their working years.
Technology startups with young, dual-income workforces commonly have many employees covered under both their own employer plan and their spouse's plan. These companies benefit from clear communication about the birthday rule for dependent children. Tech companies often use modern HRMS software to help employees model different scenarios and choose the most cost-effective coverage combination for their families.
Implementation Plan: Setting Up Effective Dual Coverage Management
Creating a systematic approach to coordination of benefits protects both your organization and your employees:
Month One: Audit Current Processes.
Review how your organization currently handles coordination of benefits information. Check your enrollment forms, HRIS systems, and HR team knowledge. Identify gaps in documentation, training, or procedures. Survey employees to understand their confusion points and common questions.
Month Two: Build Educational Resources.
Create clear, simple materials explaining coordination of benefits. Include flowcharts showing how claims move from primary to secondary insurance. Write FAQs addressing the most common questions. Develop decision tools helping employees determine if secondary coverage makes financial sense. Make everything available in your employee portal.
Month Three: Train Your HR Team.
Conduct comprehensive training on coordination of benefits rules. Cover the birthday rule, Medicare coordination, COBRA as secondary, and state-specific requirements. Provide your team with quick reference guides they can use when answering employee questions. Role-play common scenarios to build confidence.
Month Four: Update Systems and Forms.
Modify your HRIS to properly track coordination of benefits information. Update enrollment forms to collect complete secondary insurance details. Add fields for spouse coverage, Medicare eligibility, and other relevant data. Configure your system to flag when employees might have coordination issues.
Month Five: Launch Employee Education Campaign.
Roll out your new educational materials during open enrollment. Host webinars and benefit fairs where employees can ask questions. Send targeted communications to specific groups who need coordination of benefits guidance, like employees approaching Medicare age or those recently married. Make coordination of benefits education part of your standard employee onboarding process.
Month Six and Beyond: Monitor and Improve.
Track common questions and problems related to dual coverage. Review claim denials related to coordination of benefits. Gather feedback from employees about what remains confusing. Update your materials and processes based on what you learn. Make coordination of benefits a standing agenda item in quarterly HR team meetings.
Future Outlook and Trends: Evolving Insurance Coordination
Several trends will reshape how businesses handle primary and secondary insurance in coming years:
Technology integration will automate more coordination of benefits processes. Modern HRIS platforms increasingly connect directly with insurance carriers to verify coverage and coordinate benefits electronically. This reduces manual work for HR teams and speeds up claim processing. Expect artificial intelligence to help identify coordination issues before they cause claim denials.
Medicare eligibility age changes could alter coordination rules. As discussions continue about raising the Medicare eligibility age or creating Medicare buy-in options for younger workers, coordination of benefits rules will need updating. Forward-thinking employers should monitor these policy discussions and prepare for potential changes.
Transparency requirements will increase. More states are passing laws requiring clear disclosure of coverage options and costs. This trend will extend to coordination of benefits, with employers needing to provide clearer information about how multiple plans work together. Organizations that get ahead of these requirements will have smoother compliance paths.
The growth of high-deductible health plans combined with Health Savings Accounts creates new coordination complexities. When employees have HDHPs as either primary or secondary insurance, special rules apply. Understanding these nuances becomes more important as HDHPs gain market share.
The future belongs to organizations that view benefits coordination as strategic rather than administrative. Companies that invest in proper systems, training, and employee education will see higher satisfaction, lower administrative costs, and fewer compliance issues. As dual coverage becomes more common, mastering coordination of benefits shifts from a nice-to-have skill to a must-have capability for competitive employers.
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Keep Reading
Key Elements of an Effective Manufacturing Onboarding Checklist: Complete Guide for HR Leaders
"Safety first isn't just a slogan—it's a survival strategy."
Top 9 Manufacturing Onboarding Software Features: Safety, Mobile-first, and More
Tell me the truth: that onboarding software your company has been using to onboard your
Manufacturing Employee Onboarding Software: Automate New Hire Training with Digital Workflows and Compliance Management
TL;DR: Manufacturing employee onboarding software reduces new hire time-to-productivity
Ready to streamline your onboarding process?
Book a demo today and see how HR Cloud can help you create an exceptional experience for your new employees.

