ASO Benefits
- Why ASO Benefits Matter for Strategic Business Management
- Core Components of ASO Benefits Programs
- ASO Benefits Compared to Alternative Models
- Implementing ASO Benefits Successfully in Your Organization
- Common ASO Benefits Mistakes That Create Problems
- How Different Industries Apply ASO Benefits
- Building Your ASO Benefits Program Step by Step
- Emerging Trends Reshaping ASO Benefits Administration
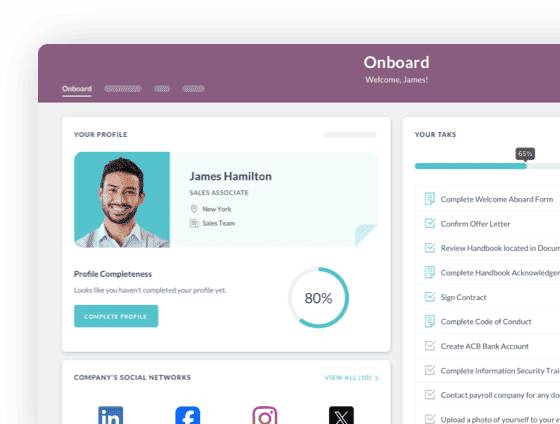
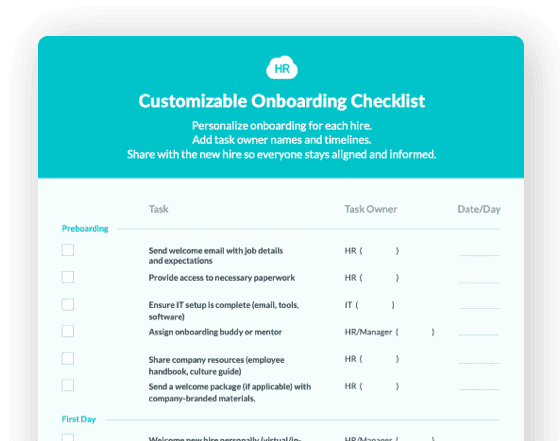
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
ASO benefits, or Administrative Services Only benefits, represent a strategic outsourcing arrangement where organizations retain ownership and financial responsibility for their employee benefit programs while delegating administrative tasks to a third party provider. This model gives you the best of both worlds: maintaining control over your benefits administration strategy while freeing your team from the time consuming complexities of daily benefits management. Unlike fully insured plans where insurance carriers assume financial risk, or Professional Employer Organizations that create co employment relationships, ASO arrangements keep you firmly in the driver's seat as the employer of record.
The ASO model addresses a critical pain point for growing businesses. As your workforce expands beyond 50 to 100 employees, benefits administration becomes increasingly complex. Compliance requirements multiply, employee questions consume HR bandwidth, and administrative errors create expensive problems. You need professional support but don't want to surrender control over benefit decisions, carrier relationships, or your employment practices. ASO benefits solve this dilemma by providing expert administration without the co employment complications that come with other outsourcing models.
Organizations across all industries use ASO arrangements to manage health insurance, dental and vision plans, life insurance, disability coverage, flexible spending accounts, health savings accounts, COBRA continuation, retirement plans, and leave of absence programs. The ASO provider handles enrollment, eligibility verification, premium reconciliation, claims support, compliance reporting, and employee communications. According to the Society for Human Resource Management, companies engaging HR outsourcing firms save money, focus more on strategy, and improve compliance with federal and state regulations. This strategic approach transforms benefits from an administrative burden into a competitive advantage.
Why ASO Benefits Matter for Strategic Business Management
Implementing ASO benefits delivers tangible advantages that extend far beyond simply reducing paperwork. Organizations that leverage this model create efficiencies that directly impact their bottom line and competitive positioning.
First, ASO arrangements significantly reduce administrative burden on internal teams. Benefits management consumes enormous HR bandwidth through enrollment periods, qualifying life events, compliance reporting, premium reconciliations, and constant employee questions. When you outsource these tasks to ASO specialists, your team reclaims hundreds of hours annually for strategic initiatives like talent development, culture building, and workforce planning. This efficiency gain becomes even more valuable as your organization scales.
Second, ASO benefits provide access to specialized expertise without the cost of full time staff. Benefit regulations change constantly at federal, state, and local levels. COBRA notices, HIPAA privacy requirements, ACA reporting, ERISA compliance, and state continuation coverage each demand specific knowledge. ASO providers maintain teams of specialists who track regulatory changes, implement updates, and ensure your programs meet all requirements. This expertise protects you from costly compliance violations that can reach thousands or even millions of dollars.
Third, ASO arrangements maintain employer control and flexibility. Unlike PEO models where you must use the provider's benefit carriers and plans, ASO allows you to select and negotiate directly with insurance companies, maintain existing broker relationships, and design benefit programs that fit your workforce demographics and budget. This control matters tremendously when you've built strong carrier partnerships or need specialized coverage options.
Fourth, the model improves benefits accuracy and employee experience. ASO providers use sophisticated HRIS platforms that integrate with payroll systems, reducing data entry errors and ensuring accurate deductions. Employees gain access to professional benefits counselors who answer questions promptly and help them maximize their coverage. This improved experience directly impacts retention and satisfaction.
Core Components of ASO Benefits Programs
Understanding what ASO arrangements typically include helps you evaluate providers and structure agreements that meet your specific needs. These components work together to create comprehensive administrative support.
Enrollment Administration:
The ASO provider manages annual open enrollment campaigns, new hire benefit elections, qualifying life event changes, and dependent verification processes. They create communication materials, host informational sessions, process election forms, and ensure accurate data transfer to carriers.
Eligibility Management:
Tracking who qualifies for benefits based on hours worked, employment status, waiting periods, and other criteria requires constant monitoring. ASO providers maintain eligibility records, process status changes, and communicate with employees about coverage effective dates and termination.
Premium Reconciliation and Billing:
Matching employee contributions against carrier invoices involves complex calculations across multiple plans and employee classes. ASO administrators reconcile premium charges, identify discrepancies, work with carriers to resolve billing errors, and coordinate payment processing.
COBRA Administration:
Federal and state continuation coverage requirements impose strict notice deadlines and complex qualification rules. ASO providers handle all COBRA processes including qualifying event notifications, premium collection, coverage termination, and documentation retention for compliance audits.
Compliance Reporting:
Benefits programs trigger numerous regulatory filings including ACA 1094/1095 forms, 5500 retirement plan reports, nondiscrimination testing, HIPAA privacy certifications, and various state mandated notices. ASO providers prepare these filings, manage deadlines, and maintain audit documentation.
Employee Communications and Support:
Questions about coverage, claims, and benefits changes arrive constantly. ASO providers staff dedicated support lines, respond to inquiries, explain benefit options during life events, and educate employees about maximizing their programs.
Technology Platform Access:
Most ASO arrangements include web portals and mobile apps where employees view coverage details, access ID cards, submit election changes, and find benefits resources. These platforms integrate with your existing HRIS and payroll systems for seamless data flow.
ASO Benefits Compared to Alternative Models
|
Feature |
ASO Benefits |
PEO Model |
Fully Insured |
Fully Self Administered |
|
Employer of Record |
You remain employer |
PEO becomes co employer |
You remain employer |
You remain employer |
|
Benefit Plan Selection |
You choose carriers and plans |
PEO's master plans |
Insurance carrier plans |
You design completely |
|
Financial Risk |
You assume claim risk |
PEO assumes some risk |
Carrier assumes risk |
You assume claim risk |
|
Administrative Burden |
Provider handles admin |
Provider handles admin |
Mix of carrier and you |
You handle everything |
|
Control Over Strategy |
Full control maintained |
Shared control |
Limited control |
Complete control |
|
Cost Structure |
Per employee fees plus premiums |
Bundled pricing |
Fixed premiums |
Internal staff costs |
Implementing ASO Benefits Successfully in Your Organization
Creating effective ASO arrangements requires thoughtful planning and clear agreements that align with your organizational needs. These best practices help you maximize value while avoiding common implementation pitfalls.
Carefully assess which benefits functions to outsource versus retain internally. Not every organization needs comprehensive ASO services. Some companies benefit from outsourcing only COBRA administration or ACA reporting while handling other functions in house. Evaluate your internal capabilities, staff bandwidth, and where specialized expertise adds most value. Start with your biggest pain points rather than outsourcing everything at once.
Select ASO providers based on demonstrated expertise in your industry and company size. Benefits compliance varies significantly across sectors. Healthcare organizations face unique requirements around credentialing and medical plan administration. Manufacturers need strong workers compensation and disability management. Technology companies require expertise with equity compensation and international benefits. Choose providers with proven success serving organizations similar to yours.
Negotiate clear service level agreements with specific performance metrics. Vague commitments like "timely enrollment processing" create disputes when expectations aren't met. Define exactly what the ASO provider will deliver, including response times for employee inquiries, accuracy standards for premium reconciliation, and deadlines for compliance filings. Establish measurement methods and consequences for missed commitments.
Ensure seamless technology integration between your systems and the ASO platform. Benefits data needs to flow automatically from your HRIS to the ASO system to payroll and to insurance carriers. Manual data transfer creates errors and defeats efficiency gains. Verify that the ASO's technology integrates with your existing platforms before signing agreements. Test data flows during implementation to confirm accuracy.
Maintain strong internal benefits knowledge even while outsourcing administration. Your HR team still needs to understand benefit plan designs, eligibility rules, and compliance requirements. Outsourcing administration doesn't mean abdicating responsibility. Keep at least one internal person who can oversee the ASO relationship, answer strategic questions, and step in if provider issues arise.
Communicate the ASO relationship clearly to employees during rollout. Workers need to understand who handles what aspects of their benefits. Explain that while a provider administers day to day tasks, you remain their employer and make all coverage decisions. Provide clear contact information for ASO support resources. Address concerns about privacy and data security.
Common ASO Benefits Mistakes That Create Problems
Even well intentioned ASO implementations fail when organizations make these avoidable errors. Recognizing these pitfalls helps you maintain effective outsourcing relationships.
Assuming ASO providers handle everything without ongoing internal involvement. Successful ASO relationships require active partnership, not abdication. You need to provide timely information about organizational changes, new hires, terminations, and policy decisions. Providers can't administer benefits effectively without accurate data and responsive communication from your team.
Failing to validate ASO compliance work and filings independently. While ASO providers should handle compliance, ultimate responsibility remains with you as the employer. Periodic audits of ACA forms, COBRA notices, and other filings ensure accuracy. Don't discover compliance failures during government audits when penalties become unavoidable.
Neglecting employee education about the ASO support structure. When workers don't understand that an ASO handles certain functions, they flood internal HR with questions the provider should answer. Clear communication during implementation and ongoing reminders about where to direct different inquiries prevent frustration and wasted time.
Allowing carrier and payroll system disconnects that create reconciliation nightmares. Benefits administration requires tight coordination between multiple systems. When enrollment data doesn't match payroll deductions or carrier billing, you face angry employees and payment disputes. Insist on integrated technology and regular reconciliation processes that catch discrepancies quickly.
Choosing ASO providers based solely on price without evaluating service quality. The cheapest provider often delivers the worst results. Benefits administration errors cost far more than the difference between providers. Evaluate providers on expertise, technology capabilities, service levels, and references from similar organizations, not just fee structures.
How Different Industries Apply ASO Benefits
ASO arrangements adapt to the unique benefit needs and regulatory environments across various sectors. Here's how leading organizations leverage this model in different contexts.
Healthcare organizations use ASO benefits extensively to manage complex coverage for diverse workforce segments. Hospitals and health systems employ physicians, nurses, administrative staff, and contract workers, each with different benefit needs and eligibility rules. ASO providers handle the intricate eligibility tracking, manage multiple plan tiers, coordinate with credentialing systems, and ensure compliance with healthcare specific regulations. Many healthcare employers also use ASO arrangements for managing leaves of absence and disability programs that interact with clinical staffing requirements.
Manufacturing companies leverage ASO benefits particularly for managing multi state operations and union employee coverage. Manufacturers with facilities across different states face varying continuation coverage requirements, disability regulations, and wage attachment rules. ASO providers maintain expertise across jurisdictions and handle the complexity of administering union negotiated benefits alongside non union programs. They also manage workers compensation coordination and return to work programs that manufacturing employers prioritize.
Technology firms use ASO arrangements to administer innovative benefit packages that help compete for talent. Tech companies often offer extensive voluntary benefits, commuter programs, student loan assistance, and wellness incentives alongside traditional coverage. ASO providers help manage the enrollment and ongoing administration of these diverse offerings while the employer retains flexibility to add or modify programs as talent markets evolve.
Retail and hospitality businesses rely on ASO benefits to handle high volume, high turnover workforces where eligibility changes constantly. With many part time workers, seasonal employees, and variable hour schedules, determining benefit eligibility becomes extremely complex. ASO providers track hours worked, apply variable hour measurement periods, manage frequent status changes, and ensure compliance with ACA look back rules that retail and hospitality employers find particularly challenging.
Building Your ASO Benefits Program Step by Step
Ready to implement or optimize your ASO benefits arrangement? Follow this structured approach to create a program that delivers results while protecting your organization.
Step 1: Conduct comprehensive benefits administration assessment. Document your current processes, identify pain points, measure time spent on various tasks, and evaluate staff capabilities. This baseline reveals where ASO support adds most value and helps you build the business case for outsourcing.
Step 2: Define service scope and performance expectations. Determine exactly which functions you'll outsource and which you'll retain. Specify response times, accuracy standards, reporting requirements, and communication protocols. Clear expectations prevent disputes later.
Step 3: Research and evaluate potential ASO providers. Request proposals from multiple providers, check references with organizations similar to yours, evaluate technology platforms, and assess cultural fit. Don't select based on price alone.
Step 4: Negotiate detailed service agreements. Document all commitments in writing, including services provided, performance metrics, technology integration, data security, pricing structure, and termination provisions. Have legal counsel review agreements before signing.
Step 5: Plan thorough implementation timeline. Map out data migration, system integration, employee communication, and training schedules. Allow adequate time for testing before going live. Rush implementations create errors that undermine the entire arrangement.
Step 6: Execute coordinated rollout communications. Inform employees about the new ASO support structure, provide contact information, explain what changes and what stays the same. Use your employee engagement platform to distribute materials and answer questions.
Step 7: Monitor performance against agreed metrics. Track response times, accuracy rates, employee satisfaction, and compliance outcomes. Address issues promptly rather than letting problems accumulate. Schedule regular review meetings with your ASO provider.
Step 8: Optimize continuously based on feedback and results. Survey employees about their ASO experience, analyze metrics trends, and adjust processes that aren't working well. Effective ASO relationships evolve as your needs change and providers improve their services.
Emerging Trends Reshaping ASO Benefits Administration
The benefits outsourcing landscape continues evolving as technology advances and workforce expectations change. Understanding these trends helps you leverage ASO arrangements more strategically.
Artificial intelligence and automation increasingly power benefits administration tasks. AI chatbots handle routine employee questions, algorithms flag eligibility issues before they create problems, and machine learning identifies enrollment errors automatically. ASO providers investing in these technologies deliver faster, more accurate service than manual processes allow.
Data analytics and predictive modeling transform benefits from reactive administration to proactive strategy. Advanced ASO providers analyze utilization patterns, predict cost trends, identify risk factors, and recommend plan design changes. This intelligence helps you optimize benefit investments rather than simply administering whatever programs you've always offered.
Integrated wellbeing programs expand beyond traditional health insurance into comprehensive employee wellness. ASO arrangements increasingly include administration of mental health resources, financial wellness tools, fitness incentives, and lifestyle coaching. This holistic approach recognizes that benefits strategy affects overall workforce productivity and retention.
Consumer directed healthcare growth requires more sophisticated administration. As high deductible plans with health savings accounts become standard, ASO providers must educate employees about maximizing these arrangements, coordinate multiple account types, and ensure compliance with complex HSA and FSA rules. This educational component becomes as important as traditional enrollment administration.
The organizations mastering ASO benefits arrangements understand that outsourcing administration doesn't mean giving up control. It means strategically leveraging specialized expertise so your team focuses on benefits strategy, workforce planning, and employee experience rather than paperwork and compliance minutiae. By implementing ASO benefits thoughtfully and managing provider relationships actively, you transform benefits from an administrative burden into a strategic asset that attracts talent, controls costs, and supports your business objectives.
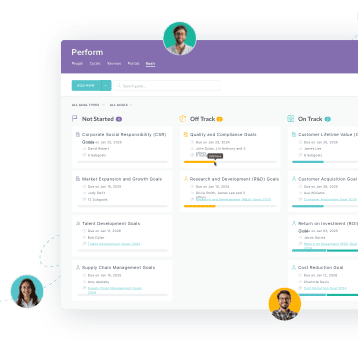
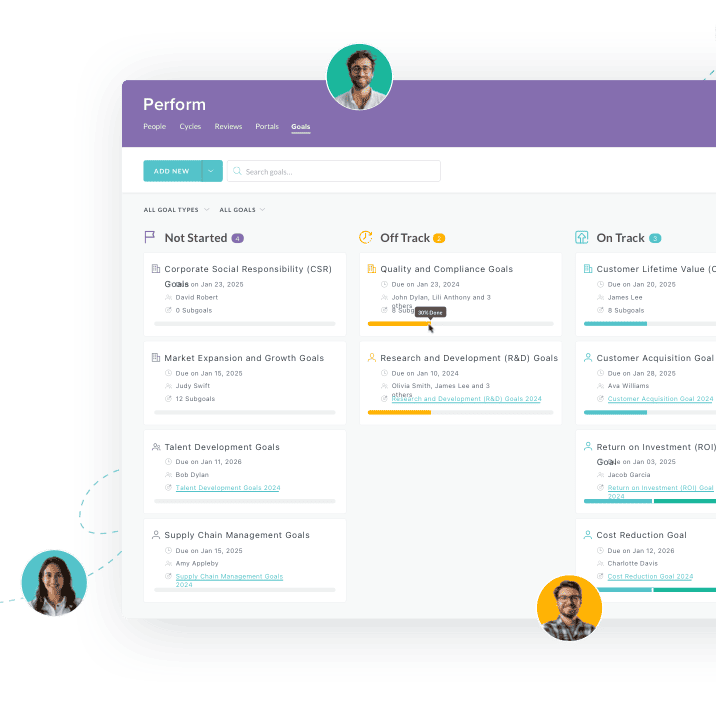
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Keep Reading
Caregiver Turnover in Home-Based Care: 5 Fixes That Actually Work
Home healthcare agencies face alarming turnover rates of 75%, with most caregivers
10 Workforce Management Issues Hospitals and Home Care Teams Face (and What Fixes Them Fast)
"We're hemorrhaging nurses faster than we can replace them, and our current systems can't
Understand The Employment Contracts: Key Legal Considerations for HR
One of the hallmarks of any successful business is a clear understanding of the
Ready to streamline your onboarding process?
Book a demo today and see how HR Cloud can help you create an exceptional experience for your new employees.

