The Definitive Guide to Onboarding Field & Clinical Staff in Healthcare (2026)
.png)
- The "Ghosting" Epidemic: Why Your New Hires Are Leaving Before They Start
- The Deskless Reality: Why Emailing PDFs to a Nurse Who Lives on Their Phone Doesn't Work
- Compliance vs. Culture: The Compass That Should Guide Every Decision
- The 4-Phase Framework: Building a 90-Day Journey That Actually Works
- What to Digitize in 2026
- The Honest Reality Check
- Where to Start This Week
- The Bigger Picture
 Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Cut onboarding time
by 60%—here's the
Ultimate Checklist
that helped do it.
Healthcare organizations lose an average of $61,110 every time a bedside RN leaves in their first year—and 20% of that turnover happens within the first 45 days. This guide provides a research-backed framework for onboarding field and clinical staff that reduces early turnover, automates compliance, and improves patient safety outcomes.
Key findings covered in this guide:
-
The turnover crisis: 58% of nurses report burnout most days, and only 39% plan to stay in their current position for 12 months
-
The mobile-first imperative: 70-80% of healthcare workers are deskless, yet most onboarding systems were designed for desktop users
-
The compliance-culture balance: How to automate OIG exclusion checks, license verification, and I-9 processing so HR can focus on mentor matching and culture-building
-
The 4-phase framework: A structured 90-day journey from pre-boarding through stay interviews that improves retention by up to 82%
-
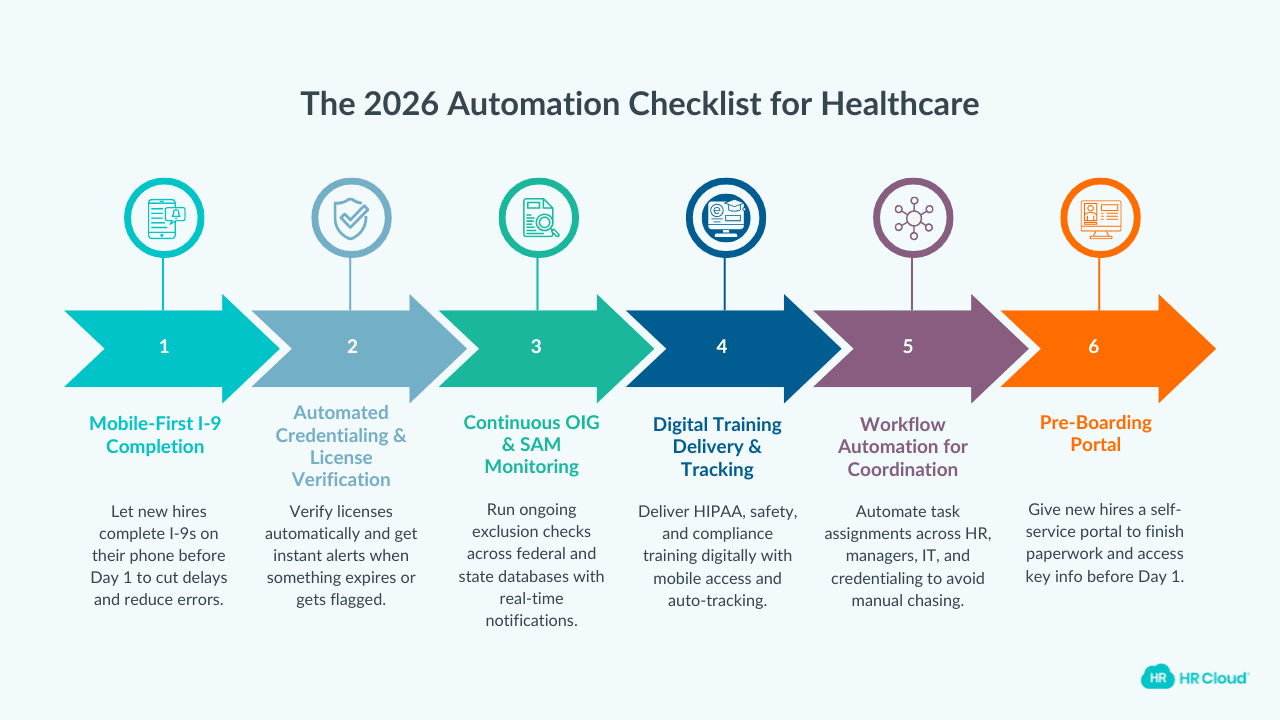
2026 automation checklist: Mobile I-9s, continuous credentialing, digital training delivery, and workflow automation priorities
This guide is designed for Hospital HR Directors, VP of People, and Operations Leaders managing clinical and field staff onboarding at scale. Research sources include Gallup, SHRM, NSI National Healthcare Retention Report, and the American Organization for Nursing Leadership.
The first 90 days determine whether your nurses stay — or start looking for the exit.
Imagine this: A highly skilled ICU nurse accepts your offer. She's exactly what you need—experienced, credentialed, ready to make an impact. But on Day 1, instead of meeting her team or learning the floor, she spends six hours in a windowless basement filling out 40 pages of forms. By noon, she's already wondering if she made a mistake.
This isn't just an "admin" problem. It's a patient safety problem. It's a retention problem. And frankly, it's a leadership problem.
Here's what I want you to know before we go any further: If your onboarding process looks anything like this, you're not alone.
Most healthcare organizations are running onboarding systems designed for a workforce that doesn't exist anymore. One where nurses sat at desks, used desktop computers, and had the luxury of time.
That world is gone. So you need to change the onboarding process before you lose the talent you fought so hard to hire.
The "Ghosting" Epidemic: Why Your New Hires Are Leaving Before They Start
Let's talk numbers for a minute because numbers have a way of convincing us of the reality better than anything else.
A 2025 survey of 2,600 nurses by Cross Country Healthcare and Florida Atlantic University found that 65% of nurses report high levels of stress and burnout. That's nearly two-thirds of your clinical workforce operating at the edge. 40% aren't sure they'd choose nursing again if given the chance.
And here's where it gets worse: according to AMN Healthcare's 2025 Survey of Registered Nurses, more than half of nurses (58%) report feeling burnout most days and only 39% plan to be in their current positions in 12 months.
The other 61%?
They're planning to change jobs, switch departments, go travel, or leave the profession entirely.
Now layer in what we know about early turnover. SHRM research confirms that up to 20% of employee turnover happens within the first 45 days of employment. Not the first year. Or the first quarter. But the first 45 days.
That means one in five of your new clinical hires are mentally checking out before they've even found the good coffee in the break room.
And when they leave?
The 2025 NSI National Health Care Retention Report puts the average cost of turnover for a single bedside RN at $61,110. For a mid-sized hospital system hiring 500 nurses a year with a 20% first-year turnover rate, that's $6.1 million walking out the door annually.
Here's my take: We've been treating onboarding as a compliance checkbox when it's actually the foundation of retention. And the data is screaming at us to pay attention.
Why Emailing PDFs to a Nurse Who Lives on Their Phone Doesn't Work
I want you to try something.
Pull out your phone. Open your email. Now try to fill out a 12-page I-9 form, upload three documents, and sign with your finger.
This is what we're asking clinical and field staff to do.
Here's a reality you need to be aware of: deskless workers—nurses, home health aides, traveling clinicians, PRN staff—represent 70-80% of the global workforce, and they're heavily concentrated in healthcare. Yet most healthcare onboarding systems were designed for people who sit at desks with dual monitors and uninterrupted time.
Research on deskless workers shows that only 40% feel connected to management, compared with much higher engagement levels among remote knowledge workers. Only 32% of deskless employees feel their organization communicates as effectively with them as with office-based staff.
That's a communication gap so wide you could literally drive an ambulance through it.
Your field clinicians are completing onboarding paperwork at 10 p.m. on their phones, sitting in parking lots between home visits. They're signing compliance documents on a 3-inch screen. They're uploading credentials through forms that weren't designed for mobile. And then your HR team is manually re-entering everything because the system didn't capture it correctly.
Think about what this actually means for your new hires.
A home health nurse covering a rural territory has maybe 15 minutes between patient visits. She's sitting in her car, eating a granola bar, and trying to complete required training modules on a system that requires a desktop browser. So she puts it off. And puts it off again. And suddenly she's getting threatening emails from HR about incomplete onboarding while she's busy actually caring for patients.
Or consider the PRN nurse picking up weekend shifts.
He's not in your building during the week. He doesn't have access to your desktop systems. He's trying to complete compliance training on his personal laptop at 11 p.m., after his kids are asleep, using a system that times out every 10 minutes.
This isn't a technology problem. It's a design philosophy problem.
Most healthcare onboarding systems were designed by people who sit at desks for people who sit at desks.
But your clinical workforce doesn't sit at desks. They're moving. They're on their feet. They're working 12-hour shifts. They're caring for patients. And when they have time for administrative tasks, that time comes in 5-minute increments, not hour-long blocks.
What if your onboarding process actually met clinicians where they are—on their phones, between shifts, in the moments they have?
What if completing onboarding felt as natural as checking a text message?
What if compliance training could be consumed in 5-minute microlearning sessions instead of 90-minute marathon PowerPoints?
Organizations that figure this out will have a significant advantage in attracting and retaining clinical talent.
And that could be your organization.
Compliance vs. Culture: The Compass That Should Guide Every Decision
Here's a framework I've found helpful when thinking about healthcare onboarding. Think of it like a compass.
Compliance is Your Magnetic North
Compliance is fixed. Non-negotiable.
You have to verify licenses, run OIG exclusion checks, complete I-9s, confirm E-Verify, ensure HIPAA training, track OSHA requirements, and document everything for the inevitable audit. Miss any of this, and you're exposed—legally, financially, and ethically.
And the stakes in healthcare are extraordinarily high. Research cited by WorkBright indicates that approximately 250,000 deaths annually are attributed to medical practice errors, and a significant portion can be traced back to insufficient credentialing processes.
One in 20 healthcare providers have negative data in their records, including potential disbarments, suspensions, and exclusions. If your onboarding process doesn't catch these issues, patients are at risk.
The OIG's List of Excluded Individuals and Entities (LEIE) is updated monthly. One-time exclusion checks at hiring aren't enough. The OIG itself recommends ongoing monitoring because individuals can become excluded after they've been hired.
Organizations that fail to continuously monitor face potential civil monetary penalties of $10,000 per item or service provided by an excluded individual, plus treble damages.
This isn't theoretical risk. Compliance violations have resulted in multi-million-dollar fines. Healthcare organizations that don't get compliance right face real financial consequences.
But here's what most organizations get wrong: they treat compliance as the entire compass.
It's not.
Compliance is magnetic north, but culture is the needle that actually guides your new hires.
Create a Culture That Supports Compliance
A nurse can be fully compliant—every credential verified, every form signed, every training completed—and still feel completely disconnected from your organization. And a disconnected nurse is a nurse who's already looking at job postings.
The organizations that get onboarding right understand this distinction.
They automate the scary stuff—the OIG checks, the license verification, the credentialing workflows—so they can focus on the human stuff. Mentor matching. Team introductions. Understanding the unit's unwritten rules. Learning who to ask when things go sideways.
Here's what the research shows: automated credentialing systems can reduce manual verification from hours to seconds. Organizations using continuous OIG exclusion monitoring eliminate the gaps that expose them to compliance violations. Digital I-9 processing cuts completion time and errors dramatically.
But here's what the research also shows: Gallup found that only 12% of employees strongly agree their organization does a great job of onboarding new employees. And employees who have an exceptional onboarding experience are 2.6 times more likely to be extremely satisfied with their organization.
The difference between "positive" and "negative" onboarding isn't whether the paperwork was done. It's whether the new hire felt welcomed, connected, and confident.
Automate compliance so you can humanize culture.
The 4-Phase Framework: Building a 90-Day Journey That Actually Works
After looking at what successful healthcare organizations do differently, I've synthesized it into a four-phase framework. It's based on what's actually working at organizations that have cut turnover significantly.
Phase 1: Pre-Boarding (Days -14 to 0) — "The Safe Landing"
The onboarding experience starts the moment someone accepts your offer—not the moment they walk through your doors.
Here's what should happen before Day 1:
Compliance automation kicks in immediately
License verification starts running. Background checks are initiated. OIG and SAM exclusion databases are queried. Credentialing workflows begin. The new hire receives a mobile-friendly portal where they can complete I-9s, tax forms, and policy acknowledgments from their phone.
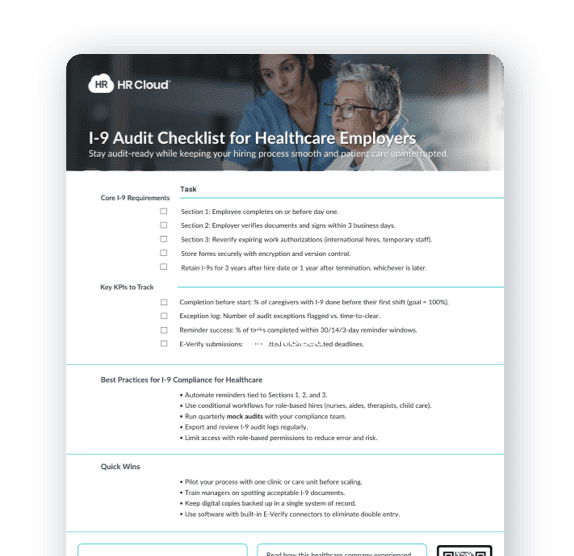
Download I-9 Audit Checklist for Healthcare Teams
The human connection begins
Their future manager sends a personal welcome message. Not a template but personalized message. Their mentor is identified and reaches out. They receive a "What to expect on Day 1" guide that actually answers their questions: Where do I park? What do I wear? Who do I meet first?
The anxiety reduction happens
New hires in healthcare often come from high-stress environments. The pre-boarding period should reduce anxiety, not increase it. This means clear communication, responsive support, and absolutely no surprises.
Research published in SAGE Journals documented one hospital that saw new-hire turnover drop from 39.1% to 18.4% after implementing a structured onboarding process with frequent touchpoints and manager communication. That's not magic. That's intentional design.
Phase 2: Week 1 — "The Connection"
The goal of week one isn't to teach everything. It's to establish connection and belonging.
Here's what matters most.
Day 1 should feel like a welcome, not an interrogation
If your new nurse spends her first day in a cubicle, filling out forms, you've already lost. Compliance documentation should be 80% complete before she walks in the door. Day 1 is for meeting people, understanding the environment, and starting to feel like part of the team.
Mentor matching happens immediately.
Not "when we get around to it." Immediately. The data on mentorship is overwhelming: research published in PMC found that structured mentorship programs had positive effects on newly graduated nurses' decision to remain in nursing, as well as on their self-confidence, problem-solving, and professional communication. American Nurse Journal reports that mentorship programs can reduce turnover by 2-15%.
The unit-level orientation matters more than the corporate one.
Yes, new hires need to understand the organization. But they need to understand their unit more:
-
Who's the charge nurse?
-
What are the unwritten rules?
-
Where do things actually get done?
Safety training should happen in context, not abstraction.
HIPAA compliance, infection control, emergency procedures—all are critical. But presenting them as day-long death-by-PowerPoint sessions is the wrong approach. Simulation training, role-specific scenarios, and mobile-accessible refreshers work better.
By the end of week one, your new hire should be able to answer: "Do I belong here?"
If the answer is "I'm not sure," you're in trouble.
Phase 3: Month 1 — "The Ramp Up"
Month one is where competence and confidence build together. This is also where many organizations drop the ball. They assume that once the initial orientation is complete, the new hire is "onboarded." Well, they're not.
Supervised practice with graduated independence.
New clinical hires shouldn't be thrown into full patient loads immediately. Preceptorship matters. Buddy systems help.
The research is clear: initial reductions in productivity during training periods contribute to 45-88% of turnover costs, but the alternative—inadequate training—contributes to adverse patient outcomes.
One approach that's working in large healthcare organizations is incrementally increasing patient loads. Because large organizations have large workforce, and they can afford to do this.
Here is a sample plan:
1. In week one, new nurses shadow and assist.
2. In week two, they take a reduced patient load with constant support.
3. By week three, they're moving toward full loads with available backup.
4. By month end, they're independent but not isolated.
Mandatory regular check-ins
30-day structured interviews with managers should be standard, not exceptional. These should not be performance reviews. They should be "How are you really doing?" conversations. Ask about challenges. Ask about support needs. Ask what's surprised them. Ask what they wish had been different about their first week.
The American Organization for Nursing Leadership reports that new hire check-ins have a powerful effect on first-year nurse retention, especially when managers have the time and bandwidth to conduct them consistently.
The challenge?
Managers are overwhelmed with administrative and operational workloads.
Executives must actively adjust those workloads to protect time for these critical conversations.
Continued compliance integration
By now, any remaining credentialing items should be resolving. License verifications should be complete. Any flags from background checks should be addressed. The compliance engine should be running in the background, not creating friction.
If there are compliance gaps at day 30, take that as a process problem, not an individual problem. Your pre-boarding should have caught these issues before they became month-one fires.
Culture reinforcement continues
Recognition should start early. New hires who receive meaningful recognition in their first month are significantly more likely to stay. Not just pizza parties but genuine acknowledgment of contributions.
A manager who notices when a new nurse handles a difficult patient interaction well—and says so—is building retention.
Research cited by HIT Consultant found that 36% of employees say consistent, frequent recognition is more important to them than a 10% pay raise. That's a powerful insight for healthcare organizations struggling to compete on compensation alone.
By the end of month one, your new hire should be able to answer: "Am I capable of doing this job?"
If they're still struggling with basics, your training process needs work.
 Ready to pass your next audit—without the stress? See how you can simplify compliance and eliminate gaps before they become problems.
Ready to pass your next audit—without the stress? See how you can simplify compliance and eliminate gaps before they become problems.
Phase 4: Day 90 — "The Stay Interview"
Here's something most organizations miss: Day 90 is as important as Day 1.
The 90-day mark is when temporary feelings become permanent decisions. It's when "I'll give it a chance" becomes "I'm committed" or "I'm starting to look."
SHRM reports that employees who experience great onboarding are 69% more likely to stay with a company for at least three years.
Conduct a formal stay interview
90-day interview should be conducted like a stay interview, not a performance review. That's a nuance you should be intentional about.
Performance reviews focus on what the employee is doing. Stay interviews focus on what will make them stay—or leave.
Ask:
-
What's working? What's not?
-
What's one thing we could do better? Is this role what you expected?
-
What would make you want to stay for five years? What would make you leave?
These aren't easy questions to ask. They require genuine openness to hearing things you might not want to hear. But organizations that conduct stay interviews—and actually respond to the feedback—see measurable improvements in retention.
Review competency and confidence
By now, your new hire should be functioning independently. If they're not, address it directly—with support, not judgment. Sometimes 90 days isn't enough for a particular role or individual. That's okay.
But you need to know where they stand and what additional support might help.
If they are functioning independently, acknowledge it explicitly. Recognition at the 90-day mark reinforces that the hard work of ramping up has been noticed.
Document everything
The 90-day milestone should be formally recognized in your systems. Training completion should be verified. Competency assessments should be documented. Compliance items should be fully closed. The new hire should transition from "new" to "team member" both culturally and administratively.
Plan for continuous development
The onboarding journey ends but the development journey continues:
-
What's next for this person?
-
What career paths are available?
-
What opportunities exist for growth, specialization, or leadership?
-
How will you continue investing in their development?
The best healthcare organizations don't treat Day 90 as the finish line. They treat it as the starting line for a longer-term relationship.
A 2025 study in Worldviews on Evidence-Based Nursing documented a mentorship program that cost approximately $4,000 to implement but resulted in avoiding approximately $480,000 in turnover costs when all mentees remained employed for minimum three months past the program. That's transformational ROI.
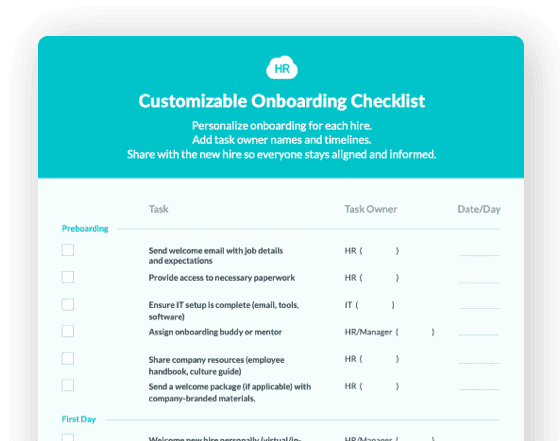
Download healthcare onboarding checklist.
What to Digitize in 2026
Alright, let's get practical. Here's what healthcare organizations should be automating in their onboarding process today.
Mobile-First I-9 Completion
I-9s are the most common source of onboarding delays and compliance violations. Mobile-first I-9 processing lets new hires complete Section 1 from their phone before Day 1, with photo document upload and electronic signature. Automated systems can reduce the traditional multi-hour manual process to minutes.
Automated Credentialing and License Verification
Primary source verification of licenses and credentials should happen automatically. Systems should connect directly to state licensing boards, continuously monitor for changes, and alert you immediately if something expires or gets flagged. Healthcare organizations using automated credentialing report reducing processing time from weeks to hours.
Continuous OIG and SAM Exclusion Monitoring
One-time exclusion checks at hiring aren't enough. The OIG recommends ongoing monitoring because individuals can become excluded after hire. Automated systems check multiple federal and state databases continuously and alert you the moment something changes. MedTrainer reports customers save 40 hours per week on average through automation.
Digital Training Delivery and Tracking
Mandatory training—HIPAA, infection control, OSHA, safety protocols—should be delivered digitally, accessible on mobile devices, and automatically tracked for completion. Look for systems that support microlearning (short, focused modules) rather than hour-long sessions.
Workflow Automation for Task Coordination
Onboarding involves multiple stakeholders: HR, the hiring manager, IT, security, credentialing, the unit, and the mentor. Automated workflows ensure tasks are assigned, tracked, and completed without requiring someone to manually coordinate everything.
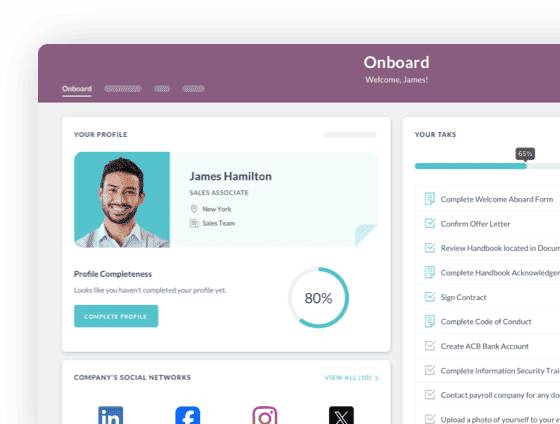
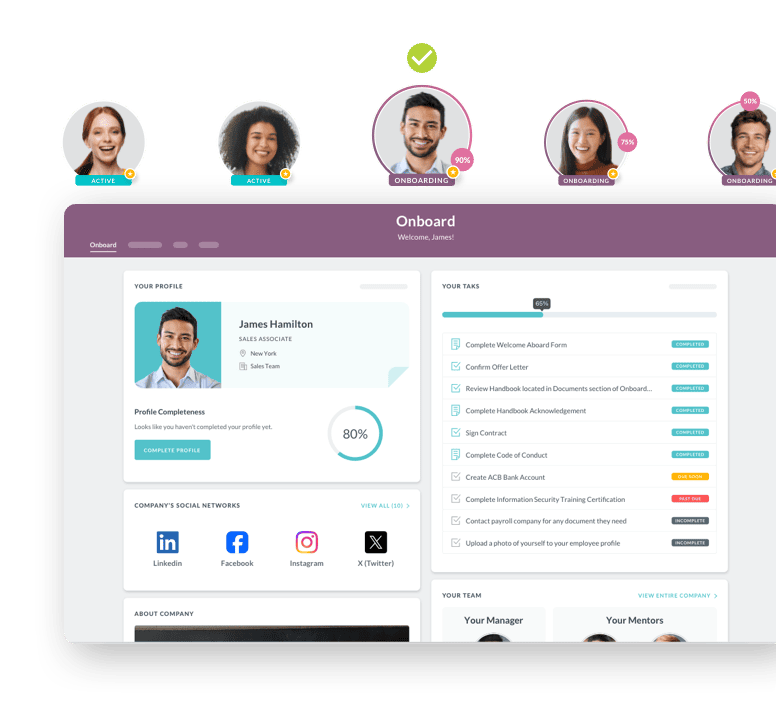
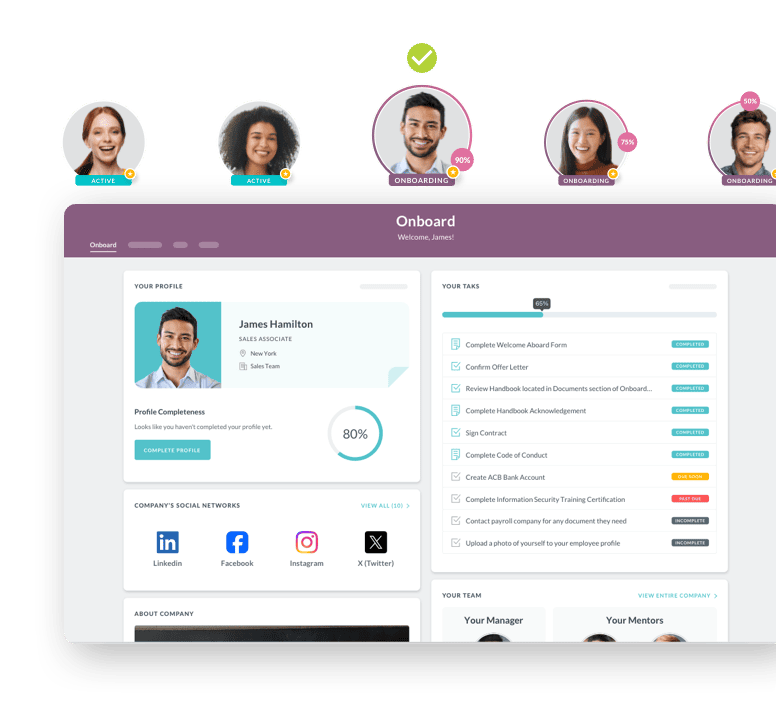
Pre-Boarding Portal
New hires should have access to a self-service portal before Day 1 where they can complete paperwork, access training materials, meet their team virtually, and get answers to common questions.
Will automation solve everything? No.
You'll still need human judgment, personal connection, and culture-building. But automation handles the mechanical, so your team can focus on the meaningful.
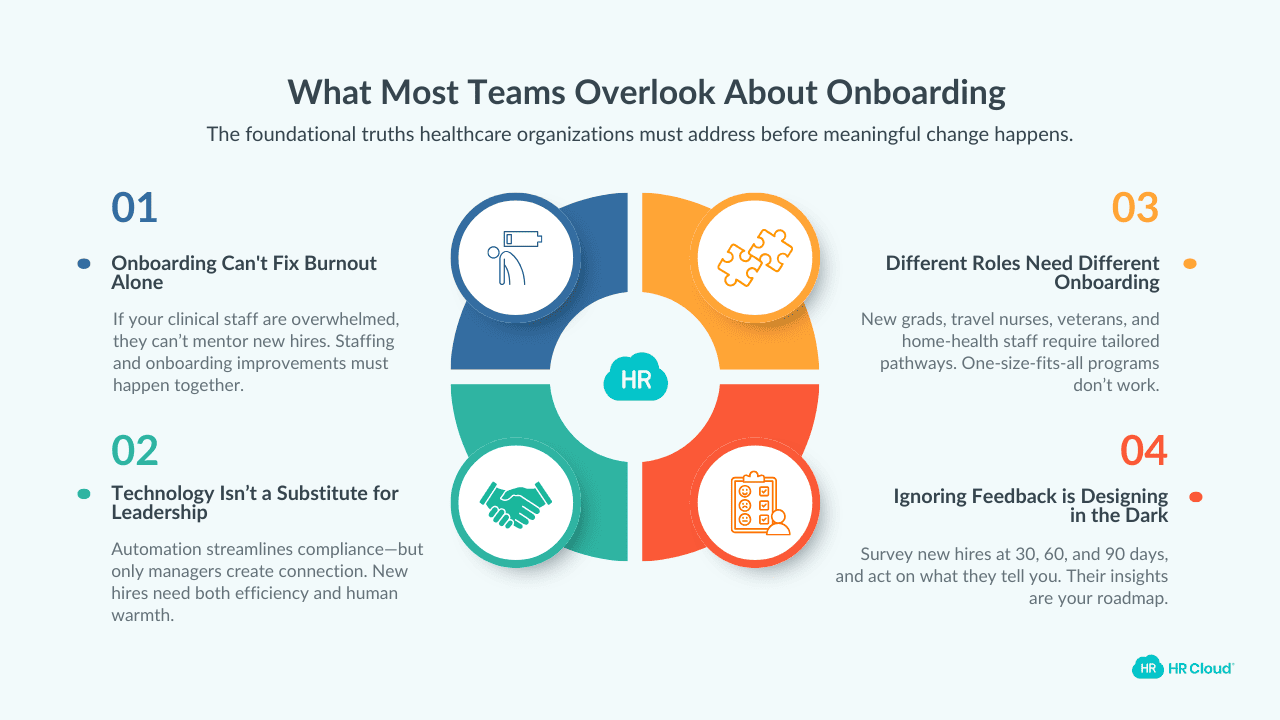
The Honest Reality Check
Here's where I need to be straight with you.
Implementing a comprehensive onboarding transformation isn't simple. It requires investment—in technology, in process redesign, in training. It requires change management, because people are comfortable with existing processes even when those processes are broken.
Some things that probably won't work:
-
Trying to fix onboarding without addressing staffing: If your existing nurses are so burned out they can't mentor new hires, no onboarding program will save you. The Hallmark Healthcare 2025 survey found that 67% of healthcare leaders cite burnout as a significant concern. Onboarding improvement and staffing improvement have to happen together.
-
Expecting technology alone to create connection: A great mobile app can streamline compliance. It cannot replace a manager who personally welcomes a new hire on Day 1. Technology enables human connection; it doesn't substitute for it.
-
One-size-fits-all approaches: A new grad nurse needs different onboarding than a 20-year veteran joining from another system. A travel nurse needs different onboarding than a permanent hire. Field-based home health staff need different approaches than facility-based nurses. Build flexibility into your framework.
-
Ignoring what your current new hires are telling you: If you're not asking new hires for feedback on your onboarding process, you're designing in the dark. Survey them at 30 days, 60 days, 90 days. And actually do something with what they tell you.
But here's what you should know: Organizations that get onboarding right don't just reduce turnover. They create competitive advantage. In a market where qualified clinical staff have abundant options, the organizations that make new hires feel welcomed, supported, and confident will win the talent war.
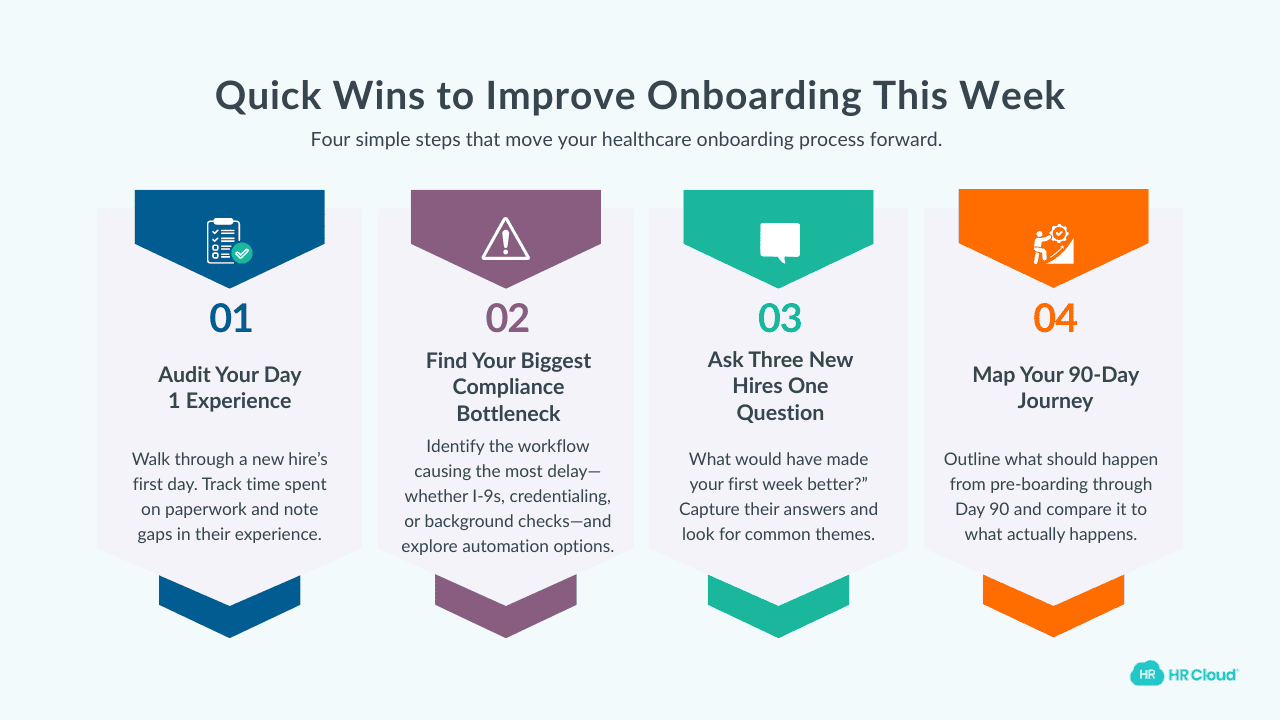
Where to Start This Week
I'm not going to pretend you can transform your entire onboarding process by Friday. But you can definitely make a start.
-
Action 1: Audit your current Day 1 experience. Walk through exactly what a new clinical hire experiences on their first day. Time how long they spend on paperwork. Note what happens—and what doesn't. Be honest about what you find.
-
Action 2: Identify your biggest compliance bottleneck. Is it I-9s? Credentialing? Background checks? License verification? Pick the one that causes the most delays and investigate automation options specifically for that process.
-
Action 3: Ask three recent hires one question. "What would have made your first week better?" Listen. Write it down. Look for patterns.
-
Action 4: Map your 90-day journey. Even if it's just on a whiteboard, map out what should happen at pre-boarding, Day 1, Week 1, Month 1, and Day 90. Compare it to what actually happens.
These aren't massive projects. They're baby steps towards developing an onboarding process your people need.
The Bigger Picture
Healthcare is facing a workforce crisis that isn't going away anytime soon. The pandemic accelerated trends that were already in motion. Nurses are tired. They're burned out. They're leaving at rates that threaten the stability of the entire system.
You cannot solve this crisis by hiring faster. The supply of qualified clinicians isn't infinite.
You solve it by keeping the people you have.
And keeping people starts on Day 1. Actually, it starts before Day 1—the moment they accept your offer and start wondering whether they made the right choice.
Onboarding isn't paperwork. It's not compliance. It's not training. It's the first chapter of a story you're writing together with every new hire. And that story either ends with "I'm building my career here" or "I should have stayed where I was."
The organizations that treat onboarding as strategic, not administrative will thrive. The ones that don't will continue hemorrhaging talent and wondering why.
You have more control over this than you might think. Use that control and act now.
For more practical guides on building onboarding systems that work for field and clinical staff, explore HR Cloud's healthcare onboarding solutions.
 Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
Discover how our HR solutions streamline onboarding, boost employee engagement, and simplify HR management
FAQs
How long should healthcare onboarding take?
Effective healthcare onboarding should span at least 90 days—not just a few days of orientation. Research shows nurses who receive structured 90-day onboarding are 69% more likely to stay three years. The first week focuses on connection and culture, month one builds competence, and day 90 confirms they're thriving and committed.
What's the difference between onboarding and orientation in healthcare?
Orientation is typically a one-time event covering policies, paperwork, and facility tours—usually completed in days. Onboarding is a strategic, ongoing process lasting weeks to months that integrates new hires into your culture, builds clinical competence, and establishes relationships. Think of orientation as the paperwork; onboarding is everything that makes someone want to stay.
How much does it cost when a nurse leaves in their first year?
The average cost of turnover for one bedside RN is $61,110, according to the 2025 NSI National Healthcare Retention Report. This includes recruiting, hiring, training, and lost productivity. For a hospital hiring 500 nurses annually with 20% first-year turnover, that's over $6 million walking out the door every year.
What compliance requirements must healthcare onboarding include?
Healthcare onboarding must include I-9 verification, E-Verify (where required), OIG exclusion list checks, state license verification, background checks, HIPAA training, OSHA safety training, and credentialing documentation. The OIG recommends continuous exclusion monitoring—not just at hire—since providers can become excluded after employment begins.
How do you onboard travel nurses or PRN staff quickly?
Travel and PRN nurses need streamlined, mobile-first onboarding that can be completed before their first shift. Prioritize digital pre-boarding with license verification, compliance forms, and unit-specific protocols accessible on mobile devices. Focus on the essentials: where to go, who to ask, and what's different about your facility. You can skip the corporate history lecture.
What is mobile-first onboarding and why does it matter for clinical staff?
Mobile-first onboarding means designing your entire process to work seamlessly on smartphones—not retrofitting desktop systems with a mobile app. It matters because 70-80% of healthcare workers are deskless; they complete paperwork between shifts, in parking lots, or at 10 p.m. on their phones. If it doesn't work on mobile, it doesn't work.
How can hospitals reduce first-year nurse turnover?
Hospitals can reduce first-year turnover by implementing structured 90-day onboarding with pre-boarding engagement, mentor matching on day one, weekly check-ins during month one, and formal stay interviews at day 90. Research shows structured onboarding improves retention by 82%. Automate compliance tasks so managers have time for the human connection that actually keeps nurses.
What should happen before a new nurse's first day (pre-boarding)?
Pre-boarding should include automated license verification, background checks, OIG exclusion screening, and digital completion of I-9s and tax forms via mobile-friendly portals. The hiring manager should send a personal welcome message, introduce the assigned mentor, and provide clear "what to expect on Day 1" guidance, including parking, dress code, and who to meet first.

Keep Reading
Onboarding Adjunct Faculty and Part-Time Instructors at Scale
Adjunct faculty teach the majority of credit hours at many institutions. They're also the
A Practical Guide to Standardizing Staff Onboarding Across Multiple University Campuses
The Medical School does it one way. The Engineering Department does it another. And the
Implement Standard Blueprint for Teacher Onboarding: Ensure Equity Across Your District
Picture this: It's the first day of the new session. Two new teachers are starting in
Like What You Hear?
We'd love to chat with you more about how HR Cloud® can support your business's HR needs. Book Your Free Demo

Build a Culture of Recognition. Boost Engagement. Guaranteed.
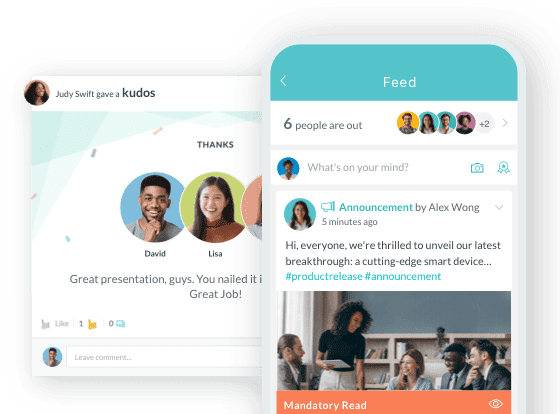
Workmates empowers employees to stay informed, connected, and appreciated—whether they’re on the front line, in the office, or remote. Recognition drives 12x higher engagement.Trusted by industry leaders in every sector




Cut Onboarding Costs by 60%.
Take the confusion and follow-ups out of onboarding with automated workflows, digital forms, and structured portals—so new hires ramp faster 3X quicker.Trusted by industry leaders in every sector




%20(1).png?width=748&height=421&name=I-9%20Infographics%20(70)%20(1).png)
%20(1).png?width=748&height=421&name=I-9%20Infographics%20(71)%20(1).png)